Using Share-FI to reveal frailty in connection with cognitive impairment
Background: Frailty is a condition in which age-related changes make older people more prone to disease and injury. Like frailty, the incidence of dementia increases with age. Studies confirm that frailty and dementia can have a reciprocal negative impact on each other.
Objective: To investigate whether the Survey of Health, Ageing and Retirement in Europe – Frailty Instrument (Share-FI), a screening tool for frailty, is suitable for revealing frailty in older people if cognition is to be taken into account.
Method: A cross-sectional study from a consent-based quality register in a geriatric outpatient clinic was conducted with 184 persons over the age of 70 who were undergoing assessment for cognitive impairment orfall risk at the outpatient clinic. We mapped physical and cognitive function using validated measurement methods. Correlations between the total score on Share-FI and various cognitive tests (Mini-mental State Evaluation [MMSE], Trail Making Test A and B, and the clock drawing test) were examined using Spearman’s correlation coefficient (rank test). Secondly, we also examined correlations between individual items in Share-FI and various cognitive tests.
Results: The majority of patients in the study were referred for assessment of dementia. A hundred people (54 per cent) were considered to be non-frail, while 84 (46 per cent) were considered to be either frail or pre-frail. The mean age was relatively similar in the three groups. There were trivial correlations between the Share-FI total score and the cognitive tests (p-values from 0.322–0.824). In relation to the individual items in Share-FI, low physical activity was associated with a poorer score on the MMSE and the clock drawing test, while abnormal appetite was associated with a poorer score on Trail Making B, but the correlations were small to moderate (p-values < 0.05).
Conclusion: The Share-FI total score as a measurement of frailty was not correlated with cognitive tests, and therefore does not appear to be particularly well suited to revealing frailty if cognition is to be taken into account.
Cite the article
Endal G, Søvde B, Terum T, Søgnen E, Andersen J. Using Share-FI to reveal frailty in connection with cognitive impairment. Sykepleien Forskning. 2023; 18(92075):e-92075. DOI: 10.4220/Sykepleienf.2023.92075en
Introduction
Both in Norway and internationally, there is an increasing number of older adults. Political guidelines indicate that older people should live as long as possible in their own homes, and older frail people are one of four prioritised groups in the National Health and Hospital Plan (1).
Frailty refers to age-related changes that make older people more prone to disease and injury, and is associated with long-term stays in institutions, hospitalisations and shorter life expectancy (2–5). The incidence of frailty gradually increases with age, and affects approximately 10 per cent of those aged 65 years and over (4, 6), and 65 per cent of those over the age of 90 (7).
Like frailty, the incidence of dementia increases with age (8). Wyller and Hem (9) emphasised the importance of identifying frailty because it indicates the need for suitable, adapted treatment.
There is no uniform definition of frailty or agreement on how to identify frailty in older people. Fried et al. (2) classify patients as frail if they meet three of the following five criteria: unintentional weight loss, self-reported exhaustion, lack of energy, slow walking speed and weak grip strength.
Fried’s phenotype model (2) only covers physical measurements of frailty, although a number of studies point out that frailty and dementia may have a reciprocal negative impact on each other (5, 10–12). Conversely, Rockwood et al.’s cumulative model (3) is more comprehensive and defines frailty as the sum of negative factors, including cognitive function.
The Survey of Health, Ageing and Retirement in Europe – Frailty Instrument (Share-FI) is a respected screening tool in both research and clinical practice. Share-FI is based on Fried’s phenotype model (2, 13), and therefore does not mention cognitive function. Share-FI has proved to be a good predictor of mortality (13).
According to Danilovich et al. (14), Share-FI is well suited to identifying persons who are frail, as they have significantly poorer scores on objective physical measurements compared with those who are considered non-frail. There is more uncertainty about the pre-frail group. A weakness of the study is that it did not include measurements of cognitive function. The same author found in a later study that, as in Share-FI, objective data can be more sensitive than self-reported data in relation to detecting frailty (15).
This concurs with findings in the study of O’Caoimh et al. (16) that compares screening tools for frailty. They found that self-reported data may be less precise, particularly among those with dementia. Newer tools used to map frailty make greater provision for the correlation between cognition and frailty (17), and it is also open to question whether these concepts actually overlap.
Share-FI was tested as a measurement of frailty at a geriatric outpatient clinic, as a step in the assessment of cognitive failure and function in those over the age of 70. On the basis of this work, we raised the question of whether Share-FI is suitable for revealing frailty in the older if cognitive impairment is also to be taken into account. As a result, we investigated whether Share-F1 scores were correlated with objective measurements of cognition.
Method
The study is based on cross-sectional data from a consent-based geriatric quality register at Førde Hospital Trust that was approved by the Trust’s data protection officer. These data were collected in the period 2016–2020. The study was conducted in line with the STROBE guidelines for observational studies.
We included 184 patients – amounting to 86 per cent of all patients assessed at the outpatient clinic for fall risk, dementia or fitness to drive. The other patients were deemed to be incapable of giving consent, and we have no demographic or clinical data on them.
The dataset was anonymised following data collection in cooperation with the data protection officer and in accordance with the information patients received prior to giving consent. Therefore, the study was not subject to notification requirements.
Variables and measurement methods
All patients were assessed by a regular team consisting of a doctor, an ergotherapist and a geriatric nurse. The doctor assessed the patients, the ergotherapist conducted cognitive tests while the geriatric nurse carried out other measurements. One person entered all the measurements in the register.
The demographic data included age (years), sex (woman, man), civil status (married/partner: yes/no) and whether the person in question was living at home (yes/no).
Frailty was investigated using Share-FI, which is based on self-reporting of symptoms and function (energy, appetite, gait, physical activity), and an objective measurement of grip strength (13). A geriatric nurse helped patients to fill in Share-FI. Grip strength was measured twice in both arms using a hand dynamometer, and the highest value was used in the analyses.
Each patient received a gender-specific Share-FI total score based on a weighted scoring system linked to the risk of mortality, and was classified as non-frail, pre-frail or frail. We based the Share-FI scores on an Excel calculator provided as an attachment in the original article (15).
Cognition was examined using the Mini-mental State Evaluation (MMSE) (18). The MMSE is a screening tool for mapping cognitive functions in connection with memory, orientation ability, language understanding and visuoconstruction. The MMSE gives a continuous score from 0–30, with the higher value representing the best score. A total score of < 24 may indicate cognitive impairment.
The Trail Making Test (TMT) A and B (19) was used to measure attention, speed and executive functioning. In TMT-A, the person must connect the numbers 1‒25 in numerical order as quickly as possible. In TMT-B, the person must connect alternating numbers and letters as quickly as possible: 1–A to 13–L. A score of ≥ 61 seconds on Trail Making A and ≥ 171 seconds on Trail Making B indicates possibly reduced cognition.
The clock drawing test (20), in which the patient draws an analogue clock showing a given time, was used to map the person’s ability to plan and use videoconstructive memory. This requires attention, understanding of numbers and semantic memory (21). The clock drawing scale is from 0–5, with the highest value as the best score, while a score of ≤ 3 indicates reduced cognition.
Body mass index (BMI) was measured by multiplying body weight in kilos by body height in metres. A BMI of < 22.5 may indicate increased risk of poorer health in older people (22). The number of drugs was defined as medications the patient took regularly, and polypharmacy was defined as ≥ 5 drugs.
The number of diagnoses was based on a list of diseases registered in the quality register: heart failure, coronary disease, hypertension, stroke, atrial fibrillation, COPD, Parkinson’s disease, depression, kidney disease and diabetes. Multimorbidity was defined as ≥ 2 diseases (23).
Gait was measured by mapping walking speed. A walking speed of < 0.8 metres per second was generally defined as low (24, 25). Grip strength in kilos was measured using a hand dynamometer, JAMAR (2). Values of < 27.5 for men and < 18 for women are often considered low in older people.
Self-reported global health was measured by a question from the population health study in Nord-Trøndelag (HUNT). The wording of the question was: ‘What is your health like now?’, with the responses ‘poor’, ‘not very good’, ‘good’, and ‘very good’ (26).
Analysis
Descriptive statistics were used to describe the sample. In order to describe continuous variables, mean and standard deviations were used, and to describe other variables, frequency (per cent) was used. The main analysis focused on whether the Share-FI score was correlated with variables indicating that frailty was linked to cognition. However, we also carried out sensitivity analyses to investigate whether the Share-FI score was correlated with variables that mostly reflect physical health (BMI, walking speed, number of drugs, number of diagnoses and self-rated health.
Spearman’s correlation coefficient was used to examine whether Share-FI was correlated with the MMSE, Trail Making A and B and the clock drawing test, followed by BMI, the number of drugs, the number of diagnoses, the walking speed test and self-rated health. We coded Share-FI as follows: non-frail = 1, pre-frail = 2, and frail = 3. The scores were adjusted for gender. Correlations of < 0.2 were considered to be so low that they had little or no practical relevance, correlations of 0.20–0.29 indicated medium relevance, while correlations of ≥ 0.3 indicated significant practical relevance (27).
We also examined whether individual questions or measurements included in Share-FI were correlated with other indicators for cognition, physical health and self-rated health, using Spearman’s correlation coefficient. Two-tailed p-values were reported as a continuous indicator of uncertainty around the results. We did not adjust for multiple testing as the four measurements of cognition in the primary analysis reflected different aspects of the same construct. The reason for this is that the remainder of the correlations were secondary analyses, and we defined the effect size values for correlations (27, 28). SPSS version 26 was used in the statistical analyses.
Results
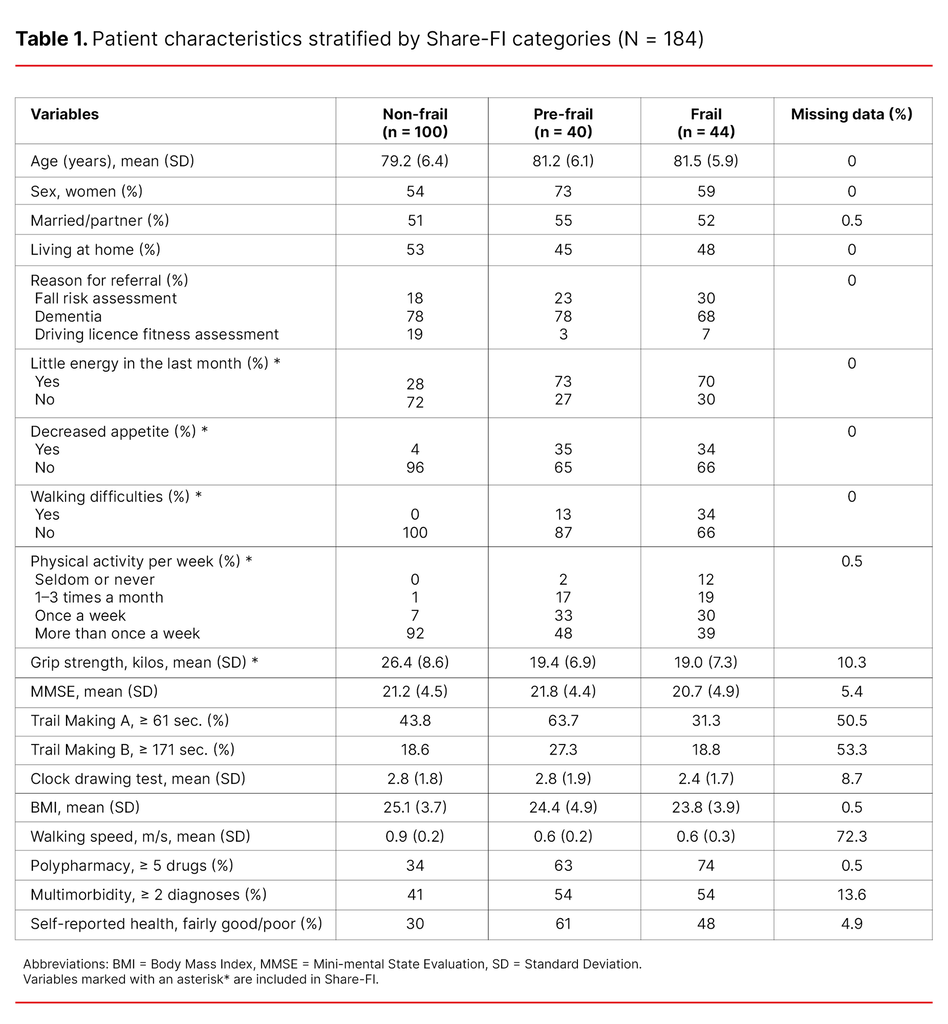
A total of 185 patients took part in the study, but one patient was excluded due to a lack of data on Share-FI. The average age was 81.2 years, and 52.9 per cent were women. Table 1 shows patient characteristics stratified by Share-FI categories.
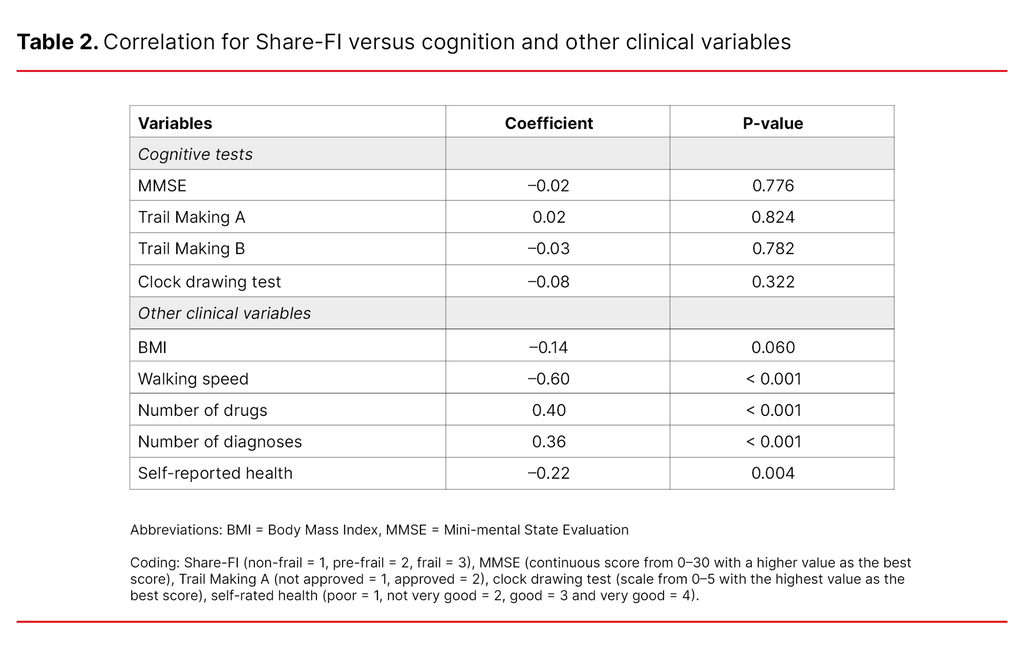
The majority of the patients were primarily referred for assessment of dementia, and classified as frail (n = 44), pre-frail (n = 40) and non-frail (n = 100). There were low and non-significant correlations between the four indicators for cognition and Share-FI (Table 2), with p-values from 0.322 to 0.824. In contrast, there were considerable significant correlations between Share-FI and walking speed, number of drugs, number of diagnoses and self-rated health (p-values < 0.05).
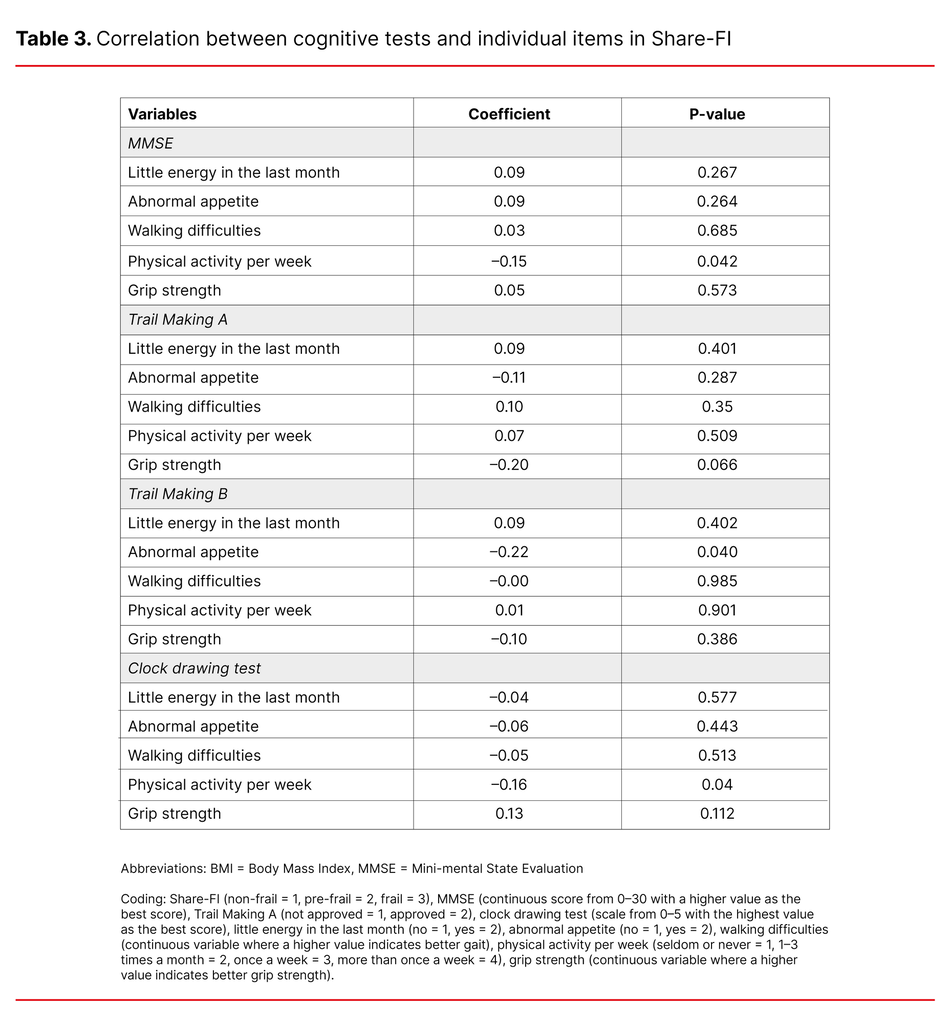
We further examined correlations between individual items in Share-FI and cognitive tests (Table 3). Of the individual items in Share-FI, low physical activity was correlated with a poorer score on the MMSE and the clock drawing test, while decreased appetite was correlated with poorer scores on Trail Making B, but the correlations were small to moderate.
Discussion
The study shows no significant correlations between the Share-FI total score and the MMSE, Trail Making A and B and the clock drawing test. Individual items in Share-FI such as low physical activity were correlated with poorer scores on the MMSE and the clock drawing test, while abnormal appetite was correlated with poor scores on Trail Making B, but the correlations were small to moderate.
The sensitivity analyses showed significant correlations between Share-FI and variables that largely reflected the physical health aspect, indicating that the participants in the study to a reasonable degree understood and answered the questions in Share-FI correctly.
Earlier research and our findings suggest that Share-FI is suitable for revealing physical frailty (13, 29). However, the primary objective of this study was to find out whether Share-FI is suitable for revealing frailty in older adults if cognition is to be taken into account. International research indicates that the concept of frailty should include cognitive impairment (10, 17, 30–32). Handajani et al. discuss the correlation between frailty and cognition, and ask whether cognitive impairment is a consequence of, a symptom of, or a driver of frailty (33).
Share-FI is frequently used to map frailty (13, 29, 32) and is constructed as a multi-dimensional index characterised by different variables pointing to a common concept, in this case frailty. The sum of the variables may show that the person in question is not frail, but it does not necessarily say so much about individual variables, i.e. the total score may be good but fails to indicate a poor score on an individual variable.
Researchers have pointed out that performing Share-FI can be challenging, particularly for those with cognitive impairment (33). Although it is possible to get help from the family to fill in the form, the self-reported responses may be unreliable, nevertheless (13).
Table 1 shows that patients who are not classified as frail generally score higher on perceived energy and physical activity. These findings concur with those of Danilovich et al. (14), who found that Share-FI distinguishes well between frail and non-frail in the case of physical function.
In contrast, the pre-frail group will need a broader assessment according to Danilovich. Neither Danilovich nor Romero-Ortuno (13) included cognitive assessment in their research. This may support doubt about the use of Share-FI in practice. This doubt is related to which tool is most suitable for revealing frailty, not to the association between cognitive function and frailty.
Share-FI is mainly based on self-reported data and may be linked to measurement errors. This might be a plausible explanation why no correlation was found between the Share-FI total score and cognitive tests in our study. Most patients who come to the outpatient clinic have incipient cognitive impairment (Table 1), characterised, inter alia, by impairment of memory and difficulty with time perspectives (21).
Patient responses may be influenced by what life used to be like, not what it is now. Self-reporting may mean a reduction in accuracy, particularly in persons with cognitive impairment (13, 16). In addition, apathy in the form of a lack of initiative, motivation and interest may entail that people have the intention of starting up activities without doing so in practice (21, p. 253).
Another possible measurement error may be overreporting of physical function and activity on the part of patients (15, 34). In recent years, user perspectives have been increasingly included in research on frailty, and Kojima et al. (5) found that some people may find it negative to be described as frail, and feel that they are being stigmatised.
An analysis of individual items and Share-FI showed more impacts in relation to cognitive tests in our study than the total score. Consequently, findings in the study of correlations between individual variables in Share-FI and cognitive tests represent an area that merits further study.
A strength of the study is that the register has an adequate sample size and uses validated measurement methods. All patients who came to the outpatient clinic were asked to participate. However, the sample consisted of patients who were under assessment and who had been referred to the geriatric outpatient clinic by their GP. There is a variation among GPs in respect of the referral rate to outpatient clinics. The outpatient clinic in our study is located in Sogn og Fjordane, which has a typical rural population, and it is uncertain whether the same results would be obtained in a different population. As a geriatric nurse helped patients to fill in Share-FI, we must show caution when comparing this with studies where no such assistance was provided.
Moreover, we used a cross-sectional study, such that we have only one measurement point, and thus cannot say anything about cause and effect. A considerable amount of data is lacking for the variables ‘Trail Making A and B’ due to the fact that this test was only carried out on a selection of patients, often in connection with a driving licence fitness assessment. The lack of data for walking speed is because this test was introduced in the course of the project. The results produced from these variables must therefore be interpreted with caution.
There is broad agreement on the importance of mapping frailty in older people, and many tools have been designed, but there is no consensus as to which is best suited (2, 4, 5). The findings in this study lead us to question the use of self-reporting as a tool to reveal frailty in persons with cognitive impairment. Individual items in Share-FI in combination with cognitive tests may give a better indication of frailty.
Older people are a heterogeneous group, and objective measurements provided the most reliable data to identify those in the process of developing frailty. Although broad geriatric assessment is frequently used to map frailty (4), it is criticised because it is time-consuming in practice. A tool for revealing frailty should be reliable and easy to use in clinical practice (5, 35).
Conclusion
The study showed no association between the total score for frailty measured by Share-FI and cognitive tests. Overall, the study does not provide grounds for concluding that Share-FI is well suited to mapping frailty if cognition is to be taken into account.
The authors declare no conflicts of interest.
Open access CC BY 4.0.
The Study's Contribution of New Knowledge
Changed from "elderly" to "older" (02.10.2023).




Comments