The ISBAR tool leads to conscious, structured communication by healthcare personnel
Students who used this framework for communication conveyed more specific observations, gave fewer unfounded opinions, and experienced improvements in teamwork and patient safety.
Background: ISBAR is a patient safety communication structure that aids simplified, effective, structured and anticipated communication between healthcare personnel. No research has previously been conducted on master’s students’ experiences of using ISBAR in Norway. In the past, there have been calls for education strategies that ensure students receive training in patient safety communication.
Objective: To elucidate specialist nursing students’ experiences of using ISBAR as a communication structure in clinical practice on a master’s degree programme in specialist nursing.
Method: The study has a qualitative descriptive design, and comprises three focus group interviews. A qualitative content analysis was carried out.
Results: Using the tool made the students’ communication more conscious, structured, clear and predictable. They conveyed objective, unambiguous and specific observations and changes instead of giving unfounded opinions. The students more readily proposed solutions of their own and clarified medical regulations. Using ISBAR made them feel more confident about their own communication and expertise, and improved their teamwork and patient safety. However, the ISBAR tool presented some challenges for the students since the communication structure had not been implemented at the hospital.
Conclusion: Using ISBAR increases the awareness of users’ own structured communication and expertise and allows them to obtain a quicker overview of patient situations. The findings highlight the importance of systematic training and simulation with the ISBAR structure in order to improve patient safety, both in the training of specialist nurses and in the specialist health service.
Teamwork and communication between healthcare personnel are vital to quality of care and patient safety (1, 2). Patient safety is defined as protection against unnecessary harm resulting from the health service’s efforts or lack of efforts (3).
Communication failures in treatment teams are one of the most common causes of adverse events in the specialist health service, and about 70 per cent are due to human errors in non-technical skills such as communication, management and decision-making (1, 4, 5). A lack of structure and standardisation is sometimes to blame for communication failures (6).
The communication structure Identify, Situation, Background, Assessment and Recommendation (ISBAR) was created to standardise the effective transfer of information in the US armed forces. ISBAR was adopted by the public health service in the 2000s (1, 7) (Table 1).
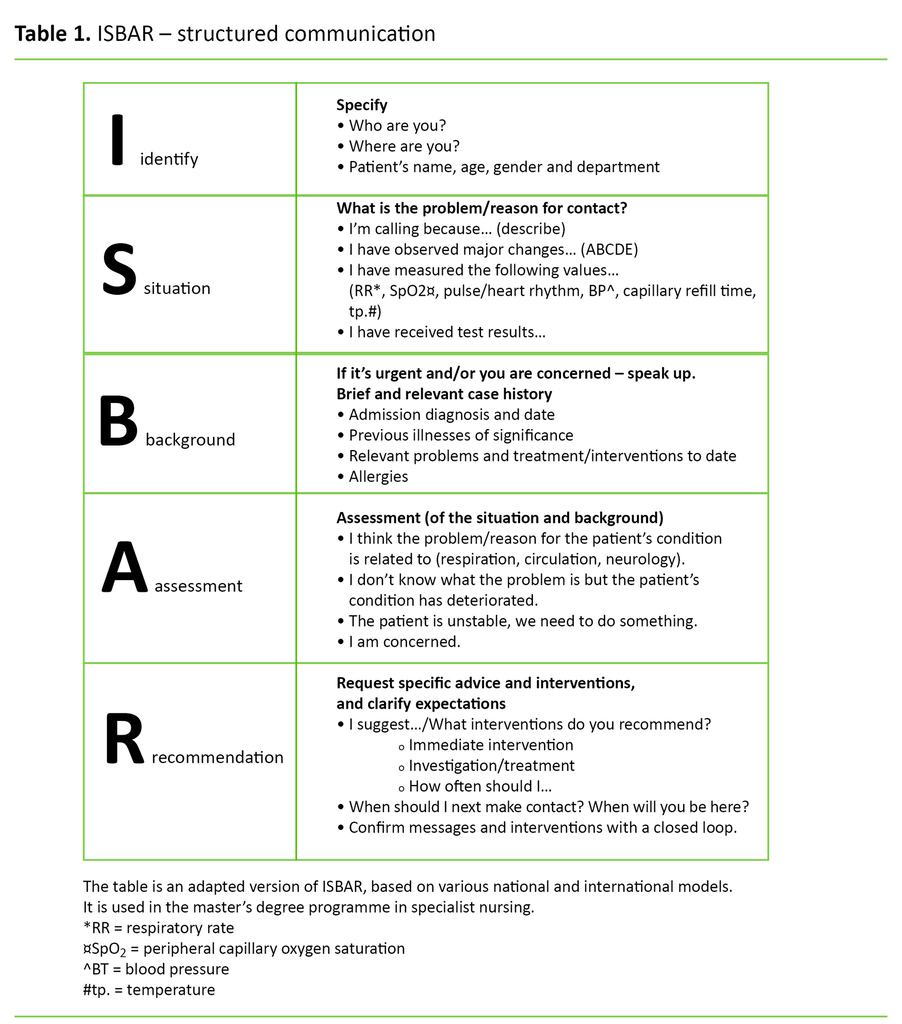
What is ISBAR?
ISBAR is one of several frameworks for communication between healthcare personnel in relation to patient situations. Use of the instrument is considered to improve patient safety through more structured, focussed and concise communication among healthcare personnel (1, 8, 9). The US healthcare system implemented ISBAR around 2003, and its overarching goal in patient safety work is to improve communication (1).
Norway introduced a national programme for patient safety in 2014 (10), but communication between healthcare personnel was not a focus area until 2017 (11). The further education programmes in paediatric and intensive care nursing recommend giving more attention to teamwork and patient safety, as well as communication and interaction with patients and their families, but team communication is not covered (12, 13).
Earlier research and the objective of the study
International studies show a reduction in unexpected deaths from 0.99 to 0.34 per thousand, as well as significant and personally experienced improvements in communication, teamwork and safety since the implementation of ISBAR (1, 14–16). Nurses found that they were better able to prioritise tasks appropriately, better prepared in general (16, 17) and better able to convey patient issues. The communication flow improved, as did the communication and interaction with the treatment team, and they felt more confident in their role (9, 14–16).
International communication training programmes and ISBAR show an improvement in observational and assessment abilities (16–19). Studies that include training in teamwork and communication using full-scale simulation show only small significant improvements compared to other teaching methods. Nevertheless, simulation is recommended for training in communication and teamwork (16, 17, 20, 21).
There is little research to confirm that theoretical skills are transferred to practice (9). Wang et al. (19) show that students want to use ISBAR in clinical practice after training. Bowling (20) calls for education strategies that ensure that students exercise patient safety in their nursing care.
No research has been found on master’s students’ experiences of using a communication structure in actual patient situations in a Norwegian context. The objective of the study is therefore to elucidate specialist nursing students’ experiences of using ISBAR as a communication structure in clinical practice on a master’s degree programme in specialist nursing.
Method
Design
The study has a qualitative descriptive design, and comprises focus group interviews.
Sample
All master’s students (n = 18) in the fourth semester of the further education programmes in paediatric and intensive care nursing were invited to participate by the management at a relevant educational institution in southern Norway. One student declined, and another was off sick on the data collection day. The total number of students who participated was therefore 16. All were women aged 27–49 with nursing experience of between 4 and 16 years.
Context
The master’s degree programme in specialist nursing included both the teaching of theory and full-scale simulation of non-technical skills (6). There was no separate training programme for the ISBAR structure, but the teaching was inspired by a training programme on communication and teamwork (22).
The first semester consisted of a two-hour resource lecture on teamwork and communication in a patient safety perspective, with ISBAR as the chosen communication structure. The students performed role plays in ISBAR communication as part of the lesson.
Between the 2nd and the 4th semester, the students completed about twelve full-scale simulations over the course of five days. ISBAR and teamwork were one of the learning outcomes. The students were encouraged to use ISBAR in clinical practice at the hospital.
Data collection
We conducted three focus group interviews in January 2016, immediately after the last simulation in the fourth semester. One focus group consisted of four paediatric nursing students, and two focus groups consisted of five and seven intensive care nursing students respectively. The first author conducted two interviews, and the third author conducted one. The second author observed the focus group interviews and acted as secretary (23).
We used an interview guide with two open-ended questions about positive experiences and challenges when using ISBAR in clinical practice. Audio recordings were made of the interviews, which were then transcribed verbatim by two of the authors. The interviews lasted between 57 and 70 minutes and were held in a meeting room at the educational institution.
Analysis
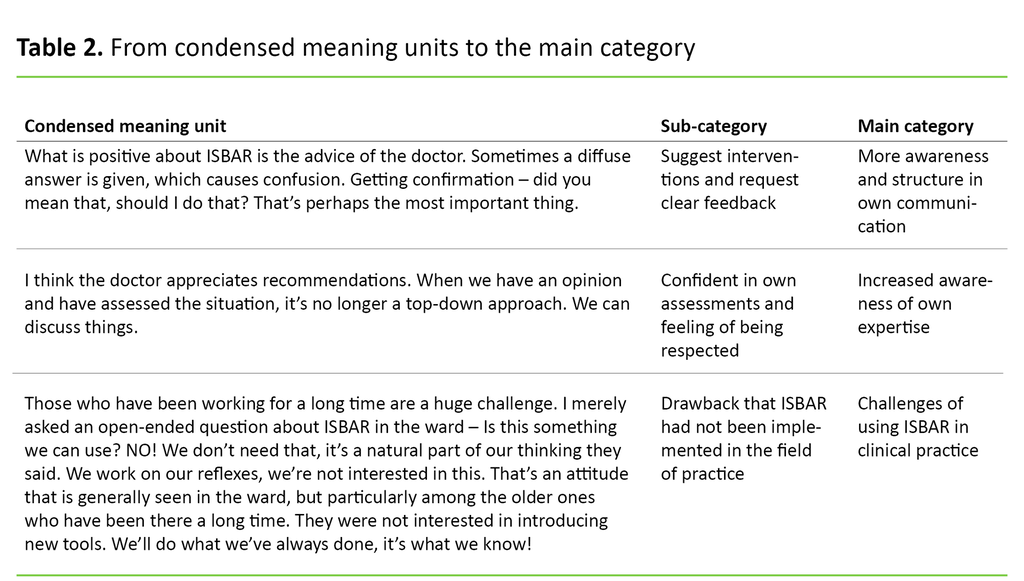
We undertook a qualitative content analysis with an inductive approach to the dataset (24). Raw data (68 pages) was read in its entirety and divided into meaning units using NVivo 11 Pro (25). Statements were condensed and systematised by content, then described and partly interpreted into subcategories and further abstracted into three main categories (24) (Tables 2 and 3). Interpretation is influenced by the researchers’ preconceptions (24).
All the authors are teachers, and three are intensive care nurses with experience from ISBAR and simulation. The results are supported by quotes from all the focus group interviews, where different voices are heard.
Ethical considerations
The study has been reported to the Norwegian Centre for Research Data (NSD) (project number 45068) and carried out in accordance with the Declaration of Helsinki’s ethical guidelines (26) on voluntary participation and anonymisation. Participants received oral and written information about the study, and all provided written consent.
Results
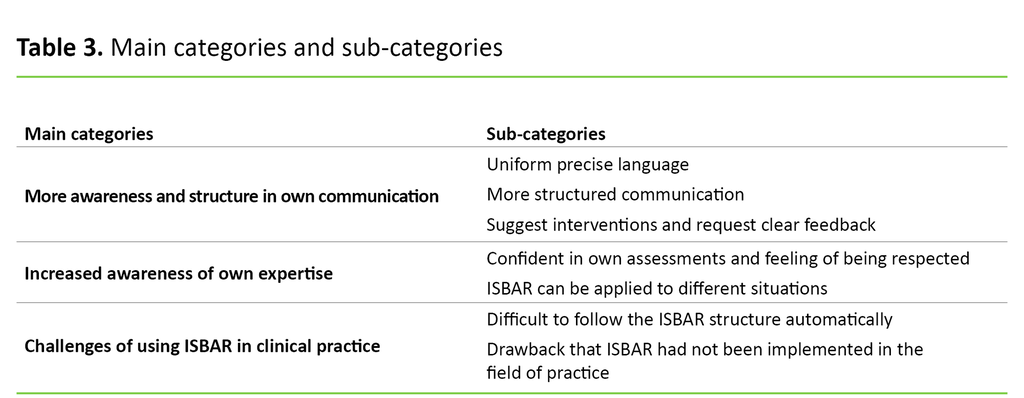
More awareness and structure in own communication
Many students had experienced that the nurse and doctor used different terminology in communication. Using ISBAR made the students more aware of the importance of uniform communication in content and language.
The students found that the patient problem was communicated more clearly and more specifically when they used ISBAR. The communication with the doctor improved, and the students found that their language had become more uniform. The students therefore felt that the teamwork had improved, and that this teamwork served as a quality assurance measure in patient treatment: ‘If we don’t have a common language between ourselves and the doctor, then the problem doesn’t get communicated… We actually communicate at a completely different level with quite a few doctors.’ (ID1-7)
Some students found the ISBAR structure to be useful, effective and time-efficient, and felt that the patient problem was communicated more swiftly: ‘Being structured certainly saves a bit of time...’ (ID1-4)
After the ISBAR training and simulation, all students agreed that structured communication was necessary. The structure and systematics of ISBAR made communication clearer and more predictable.
The students did not forget important information, and this made them feel more secure. They also conveyed patient problems in a more objective manner. When the students provided information, they focused on specific observations and changes instead of unfounded opinions: ‘ISBAR helped to make things more concrete. You describe what the problems are as opposed to what you yourself feel. The observations that emerge are more objective.’ (ID1-1)
The students agreed that ISBAR had made it easier for them to propose their own solutions for patient treatment. They all said that ISBAR had also made them aware of how important it was to ask for advice and clear feedback and to confirm agreements and instructions that had been drawn up. ISBAR thus became a tool that could be used to prevent misunderstandings and as a way of quality assuring the necessary information about the patients:
‘When I’m communicating with doctors, I try to confirm messages. Just yesterday, I wanted to wait to give a patient a tablet. ‘We’ll wait to give the patient the tablet,’ I suggested. ‘That’s right,’ said the doctor. I’ve never suggested interventions very consciously [to the doctor] before.’ (ID2-3)
Increased awareness of own expertise
Most students agreed that ISBAR had made them more confident in their own assessments in the communication with the doctor. Having confidence in their own assessments made them more aware of their own expertise: ‘Its structure shows that you’ve understood and have a lot of expertise. It helps make you more analytical.’ (ID1-7)
ISBAR was particularly useful for use in acute care situations because the students quickly gained an overview of the patient situation. This made them feel better prepared and able to be a step ahead if complications arose: ‘I think ahead more, think worst case scenario. ISBAR helps to develop that way of thinking.’ (ID1-7)
Several students found that when they used ISBAR, they received feedback from the doctor that their observations, assessments and solution proposals were relevant. This gave them a good sense of mastery, and made them feel that they had gained the respect of the doctors. They discovered through this that their own expertise was useful input to patient treatment.
Using ISBAR provided more scope for professional discussions, which led to agreement on treatment and further plans for the patient. The students found that using ISBAR resulted in good teamwork and improved patient safety: ‘I think the doctor appreciates recommendations. When we have an opinion and have assessed the situation, it’s no longer a top-down approach. We can discuss things.’ (ID3-2)
It was widely agreed that the ISBAR structure was important for all nurses, but particularly for newly qualified nurses. Some students believed that experienced nurses were able to convey the necessary information without using a fixed communication structure.
However, the students were uncertain whether it was ISBAR that had made them feel more secure in their own assessments, or if it was because their expertise had improved: ‘You learn more if you study for two years, and that impacts on the content of my assessments in ISBAR.’ (ID3-3)
Several students also had positive experiences with using ISBAR in oral reporting and written documentation. This applied to communication between nurses, during patient transfers and doctor’s rounds, and in the communication with patients’ families: ‘I also use ISBAR when I report to other departments, when we have a patient who is to be moved, or for reporting in general.’ (ID3-1)
Challenges of using ISBAR in clinical practice
Although most students thought that the ISBAR structure was useful in acute care situations, some found it difficult to follow the structure ‘automatically’ because ‘it takes many years to master it’ (ID3-2). Another challenge was that the students focused more on the sequential order in ISBAR than on the content to be conveyed, which slowed them down.
The students felt it was important to focus on ISBAR at an early stage in health studies in order to receive enough training. The importance of high-volume simulation training was emphasised: ‘It’s great that we have ISBAR in every simulation. I felt after perhaps the fourth or fifth time, yes, this is working.’ (ID2-4)
The students found that the doctors could be impatient and that they interrupted them when the students were conveying information about patient situations in accordance with the ISBAR structure: ‘[It’s a] drawback if the doctor is not familiar with ISBAR and is wondering if the nurse will get to the point soon.’ (ID2-1)
Some students said that it was sometimes difficult to suggest their own solutions and elicit a response to them, particularly from new doctors: ‘This can be a problem with new doctors if they feel undermined by the nurses’ assessments and suggestions.’ (ID3-1)
Most of the students found that they often used ISBAR during the doctor’s rounds, during telephone contact with the doctor and in nursing reports. Some students said that they used ISBAR subconsciously, while others had hardly used ISBAR at all, but wanted to do so. The students found it a drawback that the ISBAR structure had not been implemented and was not known throughout the hospital. Some students received comments such as: ‘I’ve never heard of that before...’ (ID1-2).
They feared, however, that it would be difficult to implement a fixed communication structure for experienced nurses who believed that their communication was already structured and protected patient safety: ‘Those who have been working for a long time are a huge challenge. They want to do what they’ve always done, it’s what they know.’ (ID1-7)
Since ISBAR was not implemented at the hospital in question, the students talked about different ways of implementing ISBAR. They all agreed that ‘ISBAR is here to stay’ (ID3-2).
Several suggested holding a workshop with a focus on ISBAR as a communication structure. They all believed that simulation was a suitable method for learning and using the ISBAR structure. Simulation can provide training and direct feedback on the language, content and structure of the communication: ‘Using ISBAR at a workshop. You practice [and can] use it in simulation situations, so all colleagues take part in communication training. I think that’s the way to learn it.’ (ID1-7)
Discussion
More awareness and structure in own communication
All the students found that the communication was better structured and the content was more specific when they used ISBAR. They were more conscious about conveying key, objective information about patients, and there were no linguistic misunderstandings. Uniform terminology can play a role in preventing misunderstandings and communication failures (1, 5).
The findings correspond to studies showing that the ISBAR structure improves both content and clarity in communication – it distinguishes between essential and insignificant information (14, 16). Nurses are also better prepared and can prioritise more easily (16, 17).
The students pointed out that the ISBAR structure was predictable; they did not forget important information, thereby saving time in acute care situations. This predictability is confirmed in research on ISBAR, and predictability and effectiveness are two of the objectives of implementing the structure (1, 8).
The students believed that the effectiveness of the tool was dependent on whether they had integrated ISBAR into their own professional practice. We interpret this to mean that the importance of repeated simulations is crucial to learning, a view that is supported by Husebø and Rystedt (6).
The students emphasised that getting advice was one of the most important elements of the ISBAR structure in terms of preventing misunderstandings and ensuring patient safety. Being more aware of the importance of asking for clear feedback and confirming agreements meant that the necessary information about the patient was quality assured. It is interesting to note that earlier research does not pinpoint receiving advice as one of the most important features of the ISBAR structure, but discusses clarity in general terms in all the factors of the structure (20).
Increased awareness of own expertise
Greater confidence in their own assessments and analyses, and an increased sense of mastery were prominent findings. The students found it easier to obtain an overview of the patient situation and were ready to deal with potential problems. Other studies confirm that using ISBAR improves observational and assessment abilities and self-confidence, and facilitates decision-making (9, 17).
The students felt that they received more respect from doctors when they used ISBAR. This led to more professional discussions, which resulted in agreement on treatment strategies. Professional discussions and respect from doctors supported and strengthened their expertise and sense of security in their practices. The students also found that ISBAR encouraged good teamwork and ensured patient safety in the nursing. These findings are in keeping with other studies (18).
The students reported that the ISBAR structure, together with increased expertise through the training, made them more analytical and inspired them to voice their own suggestions and reflections. The ISBAR structure also seems to represent a tool for developing clinical assessment and reasoning.
The students further found that ISBAR was useful in various reporting contexts and in communication with patients’ families. This may indicate that the students have subconsciously integrated ISBAR into their professional practice, and that they use ISBAR in various situations. Research shows that ISBAR is also used in the context of reporting and doctors’ rounds (14, 15), and supports the students’ experiences of being able to use ISBAR in such situations.
Challenges of using ISBAR in clinical practice
The students found that using ISBAR was time-consuming because the communication structure was not integrated into the work routine in the hospital. It also emerged that it was difficult to follow the structure automatically, despite them finding it easier after several ISBAR simulations. These findings show that high-volume simulation training is necessary.
Various studies show that classroom teaching alone leads to little change in communication, while a significant improvement in the nursing students’ communication can be seen through both the teaching of theory and simulation (21, 27). A meta-analysis showed that simulation had a significant impact compared to other learning strategies (21).
These findings and other research support recommendations for the closer integration of theoretical and clinical components in nursing education programmes, and for a greater focus on clinical reasoning than on critical thinking in the study programme (17).
The students were often interrupted by doctors who were not familiar with ISBAR. Some found that certain doctors did not allow a dialogue in which the students could convey their own assessments. A systematic literature review shows that different modes of communication, offensive behaviour and culture are barriers to effective nurse-doctor communication (28), and confirms the experiences of the students.
An important leadership skill in teamwork is listening to input, and obtaining and disseminating information (2, 29). Using ISBAR alone is not enough to foster good teamwork. Human factors, management and a patient safety culture are important prerequisites for teamwork and patient safety. Attention to improving non-technical skills, interprofessional collaboration and team performance where everyone can have their say are also crucial factors (29).
The students found it difficult to apply the ISBAR structure in a field of practice that had not implemented ISBAR. The Norwegian Patient Safety Programme lacks a clear focus on safe communication and has therefore not been prioritised at a number of hospitals. It was not until 2017 that ISBAR was mentioned in the care bundle for hospitals concerning early detection of deterioration in a patient’s condition (11).
Whether it is appropriate for the students to apply ISBAR in clinical practice when the field of practice has not implemented the communication structure is debatable. However, one positive aspect is that the students gain experience in introducing new knowledge on patient safety to the field of practice. It will raise students’ awareness and make them more knowledgeable about relevant quality measures. Patient safety will also improve through the use of knowledge-based practices and students will represent a useful resource in future implementation processes (12, 13, 30).
Students feared it might be a challenge to implement ISBAR with experienced nurses who showed little interest or willingness to change their own communication structure. However, the students used ISBAR to varying degrees, and some used the structure subconsciously. These findings seem to have similarities with the challenges of implementing knowledge-based practices (30) and support the fact that theoretical skills are not always transferred to practice (9).
The students suggested workshops where doctors and nurses were taught theory and carried out interdisciplinary simulations. In simulations, healthcare personnel can receive specific feedback on what they are actually saying, and not just on what they think they are saying. Communication and team training are key factors for creating and maintaining a safety culture (22, 29).
Methodological considerations
The study is important as no corresponding studies have been conducted in Norway. The authors expected the sample population to be well-informed and to have a large potential to shed light on the subject of the study (23). The study has between four and seven female respondents in each focus group, which is in line with recommendations (23, 24).
Homogeneity can strengthen the group dynamics through recognition of associative effects and past common experiences. The absence of male participants may be a weakness of the study. There were numerous congruent findings in the data collected, which may be an indication of saturation.
The first and third authors participated in all the simulations and followed the students throughout the master’s degree programme. The first author gave the ISBAR resource lecture. The authors’ existing knowledge provided a good basis for understanding how ISBAR is applied in a hospital context.
As the interviewer was also a teacher on the master’s programme, the students may have refrained from relating their negative experiences, and answered in a way that they thought the interviewer wanted to hear. In order to reduce this risk, the second author was present in all the focus group interviews. The interviewers did not supervise the students in clinical practice, and the students were informed about the authors’ dual role as both researchers and teachers before the interviews.
Preconceptions can influence the questions and the analysis, such that certain elements might be overlooked or underestimated (24). We tried to identify the preconceptions throughout the research process by involving three of the authors in the analysis process. Others may, however, analyse and interpret the findings differently.
Conclusion
The findings of the study showed that the students became more aware of their own communication structure when using ISBAR in clinical practice. They also felt more confident about their own expertise and communication, and were able to obtain a quicker overview of patient situations. These elements led to improved patient safety.
However, the students found it a challenge to use the ISBAR structure in practice as it had not been implemented in the hospital. The findings throw light on the importance of systematic training and simulations with the ISBAR structure in order to improve patient safety, both in the training of specialist nurses and in the specialist health service.
We have not investigated the long-term effects of using ISBAR in the students’ training. It is therefore important to conduct a follow-up study of students and other healthcare personnel who have received training in ISBAR.
References
1. Stewart KR, Hand KA. SBAR, communication, and patient safety: An integrated literature review. (CNE SERIES). Medsurg Nurs. 2017;26(5):297.
2. Ballangrud R, Husebø SE. Strategier og verktøy for teamtrening. In: Aase K, ed. Pasientsikkerhet: teori og praksis. 2. ed. Oslo: Universitetsforlaget; 2015. p. 248–62.
3. Saunes IS, Svendsby PO, Mølstad K, Thesen J. Kartlegging av begrepet pasientsikkerhet. Oslo: Nasjonalt kunnskapssenter for helsetjenesten; 2010. Available at: https://www.fhi.no/globalassets/dokumenterfiler/notater/2010/notat_2010_kartlegging-av-begrepet-pasientsikkerhet_v2.pdf(downloaded 13.12.2018).
4. St.Pierre M, Hofinger G, Simon R, Buerschaper C, SpringerLink. Crisis management in acute care settings: Human factors, team psychology, and patient safety in a high stakes environment. 2. ed. Berlin: Springer; 2011.
5. Helsedirektoratet. Årsrapport 2017: Meldeordningen for uønskede hendelser i spesialisthelsetjenesten. Oslo: Helsedirektoratet; 2018. Available at: https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/1446/Arsrapport2017_Meldeordningen.pdf(downloaded 14.06.2018).
6. Husebø SE, Rystedt H. Simulering innen helsefag. In: Aase K, ed. Pasientsikkerhet: teori og praksis i helsevesenet. Oslo: Universitetsforlaget; 2010.
7. Improvement I-IoH. SBAR technique for communication: A situational briefing model, 2013. Available at: http://www.ihi.org/resources/Pages/Tools/SBARTechniqueforCommunicationASituationalBriefingModel.aspx(downloaded 14.06.2018).
8. Sharp L. Effektiv kommunikation för säkrare vård. Lund: Studentlitteratur; 2012.
9. Buckley S, Ambrose L, Anderson E, Coleman JJ, Hensman M, Hirsch C, et al. Tools for structured team communication in pre-registration health professions education: a Best Evidence Medical Education (BEME) review: BEME Guide No. 41. Med Teach. 2016;38(10):966–80.
10. Saunes IS, Ringard Å. Hva gjøres for å bedre pasientsikkerheten? Satsinger i sju land. Oslo: Nasjonalt kunnskapssenter for helsetjenesten; 2013. Rapport 17/2013. Available at: https://www.fhi.no/globalassets/dokumenterfiler/rapporter/2013/rapport_2013_17_pasientsikkerhet_andre_land.pdf (downloaded 14.12.2017).
11. Helsedirektoratet. Tiltakspakke for tidlig oppdagelse av forverret tilstand (sykehus): Nasjonalt pasientsikkerhetsprogram I trygge hender 24-7; 2017. IS-2583. Available at: http://www.pasientsikkerhetsprogrammet.no/om-oss/innsatsomr%C3%A5der/_attachment/4084?_download=false&_ts=159f9ca912b(downloaded 14.12.2017).
12. Utdannings- og forskningsdepartementet. Rammeplan for videreutdanning i barnesykepleie. Oslo: UFD; 2005. Available at: http://www.regjeringen.no/upload/kilde/kd/pla/2006/0002/ddd/pdfv/269384-rammeplan_for_barnesykepleie_05.pdf(downloaded 14.12.2017).
13. Utdannings- og forskningsdepartementet. Rammeplan for videreutdanning i intensivsykepleie. Oslo: UFD; 2005. Available at: http://www.regjeringen.no/upload/kilde/kd/pla/2006/0002/ddd/pdfv/269388-rammeplan_for_intensivsykepleie_05.pdf(downloaded 14.12.2017).
14. De Meester K, Verspuy M, Monsieurs, KG, Van Bogaert, P. SBAR improves nurse-physician communication and reduces unexpected death: A pre and post intervention study. Resuscitation. 2013;84(9):1192–6.
15. Gausvik C, Lautar A, Miller L, Pallerla H, Schlaudecker J. Structured nursing communication on interdisciplinary acute care teams improves perceptions of safety, efficiency, understanding of care plan and teamwork as well as job satisfaction. Journal of Multidisciplinary Healthcare. 2015;8:33–7.
16. Foronda C, Gattamorta K, Snowden K, Bauman EB. Use of virtual clinical simulation to improve communication skills of baccalaureate nursing students: a pilot study. Nurse Educ Today. 2014;34(6):e53–7.
17. Darcy Mahoney AE, Hancock LE, Iorianni-Cimbak A, Curley MA. Using high-fidelity simulation to bridge clinical and classroom learning in undergraduate pediatric nursing. Nurse Educ Today. 2013;33(6):648–54.
18. Shin H, Kim M. Evaluation of an integrated simulation courseware in a pediatric nursing practicum. J Nurs Educ. 2014;53(10):589–94.
19. Wang W, Liang Z, Blazeck A, Greene B. Improving Chinese nursing students’ communication skills by utilizing video-stimulated recall and role-play case scenarios to introduce them to the SBAR technique. Nurse Educ Today. 2015;35(7):881–7.
20. Bowling AM. The effect of simulation on skill performance: a need for change in pediatric nursing education. J Pediatr Nurs. 2015;30(3):439–46.
21. Hegland PA, Aarlie H, Strømme H, Jamtvedt G. Simulation-based training for nurses: Systematic review and meta-analysis. Nurse Educ Today. 2017;54:6–20.
22. Agency for Healthcare Research and Quality R, MD. AboutTeam STEPPS® 2017. Available at: https://www.ahrq.gov/teamstepps/about-teamstepps/index.html(downloaded 30.10.2017).
23. Malterud K. Fokusgrupper som forskningsmetode for medisin og helsefag. Oslo: Universitetsforlaget; 2012.
24. Kvale S, Brinkmann S, Anderssen TM, Rygge J. Det kvalitative forskningsintervju. 2. ed. Oslo: Gyldendal Akademisk; 2009.
25. QSR International. NVivo 11 pro for Windows. Available at: http://www.qsrinternational.com/nvivo-product/nvivo11-for-windows/pro(downloaded 27.06.2017).
26. World Medical Association. Helsinkideklarasjonen. Declaration of Helsinki – Ethical principles for medical research involving human subjects 2013. Available at: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/(downloaded 14.12.2018).
27. Kesten KS. Role-play using SBAR technique to improve observed communication skills in senior nursing students. J Nurs Educ. 2011;50(2):79–87.
28. Tan T-C, Zhou H, Kelly M. Nurse-physician communication – NDASH – An integrative review. J Clin Nurs. 2017;26(23–24):3974–89.
29. Haerkens M, Jenkins D, van der Hoeven J. Crew resource management in the ICU: the need for culture change. Annals of Intensive Care. 2012;2(1):1–5.
30. Sandvik GK, Stokke K, Nortvedt MW. Hvilke strategier er effektive ved implementering av kunnskapsbasert praksis i sykehus? Sykepleien Forskning. 2011;6(2):158–65. DOI: 10.4220/sykepleienf.2011.0098.






Comments