Use of video communication technology in the light of everyday and/or tele rehabilitation
Video communication technology used in the context of reablement / telerehabilitation can facilitate access to nursing staff in a municipality, and enable users to stay at home longer.
The proportion of elderly is growing in the Norwegian population, and will in the foreseeable future constitute the majority of the population that will have the greatest needs for municipal care. Video communication technology (VCT) used in the context of reablement / telerehabilitation can facilitate access to nursing staff in a municipality, and enable users to stay at home longer.
Objective: Generate knowledge that is transferable to Norwegian municipalities and to make use of VCT and reablement in primary care. By choosing the perspective of the patient, the care personnel and the employer, we want to present knowledge which can be transferred and used by Norwegian municipalities.
Methods: Scoping review with searches in the databases CINAHL, Science Direct and Pubmed. Analysis of 11 empirical studies was conducted.
Results: The scoping review shows that older patients (≥ 67 years), are mainly satisfied with reablement where VCT has been applied. From an employer's perspective, one should take into account that not everybody among the care personnel will be positive towards this type of service, although many studies also show relatively high satisfaction in the aforementioned group. It is essential that necessary support and training is provided to patients and care personnel, before municipalities establish such services.
Conclusion: More municipalities should try out VCT in the context of reablement / telerehabilitation. More research is needed to determine whether this type of service will function equally well in Norway, as one has experienced abroad.
Key words: Reablement, telerehabilitation, video communication technology, primary health care, scoping review
Introduction
In 2015 there were 722 741 elderly persons in Norway, that is persons aged 67 years or above (1). The proportion of elderly persons is increasing in the population and will in the foreseeable future make up a large proportion of the population. More elderly with a need for care create challenges and possible shortages of health care personnel (2). In order to maintain sustainable care services it will be necessary to solve future care challenges in a different way than we do today. According to the Ministry of Health and Care Services, the care services have a great untapped potential in using welfare technology which may give the users greater security and a better possibility for managing on their own on an everyday basis (2).
Advanced age in and of itself is frequently accompanied by unavoidable ailments for some, such as a weakening of the muscles (3). To some, a lack of strength may make them unable to walk or care for themselves. A reduction of muscle mass may also cause a weakening of stamina, which in turn may lead to passivity. The question then becomes what may best influence health and function so that more elderly manage to maintain central functions as long as possible, without care personnel having to take over these functions for them. Part of the answer is in assisted strength training, here referring to training or exercise under professional supervision. Such training yields increased muscle strength and muscular endurance and thus improved ability to perform everyday activities in older age (4).
Knowledge of what may improve the health of the elderly (4) has in many countries resulted in increased attention to “hverdagsrehabilitering” (Norwegian), “hemrehabilitering” (Swedish) (5) and what in English speaking countries is often called “reablement” (6), “active service model”, “everyday rehabilitation” or “restorative home support” (7). Ideally everyday rehabilitation shall support the older person’s own resources and participation in everyday situations. Everyday rehabilitation is further a client centred work mode, where the various professions no longer have profession specific goals. According to Swedish research, everyday rehabilitation may be just as much about developing and reclaiming functions and activities after a hospital stay as about maintaining or preventing reduction of function (5).
What is new with everyday rehabilitation is that it frequently entails a great degree of interdisciplinary collaboration, such as between ergo or physical therapists and care personnel in a municipality. This kind of interdisciplinary collaboration is often anchored in the home care services and in a common goal of furthering everyday mastery. Health care personnel from the home care services commonly assist the user in daily training according to a training programme worked out through a collaboration between user, physical therapist, ergo therapist and nurse. Everyday rehabilitation has its origin from two main sources: everyday rehabilitation in Scandinavia and in some countries outside Scandinavia (4). The Scandinavian variety has its origin in the Östersund municipality in Sweden (5). Inspired by Östersund, Fredericia municipality in Denmark developed everyday rehabilitation in 2008 (8,9).
The purpose of this study is to gain knowledge that may be transferred to Norwegian municipalities planning to implement video communication (VC) in everyday rehabilitation in the municipal care services. In such cases ergo or physical therapist and health personnel may supervise care personnel in the home of the individual user, using VC.
Our literature study, a scoping review (10), has as its point of departure research reporting a variety of experiences with telerehabilitation. A scoping review is generally less extensive than systematic literature studies. Scoping review studies have a wider focus than systematic literature studies, and this type of study is frequently based on both qualitative and quantitative studies (10).
Telerehabilitation entails technology and methods that may be used to support, intervene or facilitate everyday rehabilitation in the primary health care services (11).
In our scoping review we are particularly interested in finding out how such a treatment programme in combination with VC has been received by users (in the article used synonymously with patients), health personnel and organisations where this has been implemented and researched.
The research questions to be illuminated are the following:
- Which experiences do users have with VC technology in rehabilitation and/or everyday rehabilitation context?
- Which experiences do health personnel have with VC technology in rehabilitation and/or everyday rehabilitation context?
- Which experiences do organisations have with VC technology in rehabilitation and/or everyday rehabilitation context?
In the next paragraph we perform a conceptual analysis with a basis in literature on the chosen subject. We also introduce the concept tele-everyday-rehabilitation. We are of the opinion that this concept encompasses the very treatment methodology beneath everyday rehabilitation and use of VC technology. Next is the methodology section, listing the sources and search words used in the literature study. The result section sums up the findings based on user experiences, experiences of health and care personnel and experiences of primary health care organisations. The discussion has as its point of departure the findings and their relevance to any planning of trial projects in which the municipalities want to use this kind of technology and treatment methodology. The literature study is financed through the VRI programme in Møre and Romsdal.
Conceptual analysis
Knowledge on issues similar to the ones we address in the literature study is in the English language research literature referred to by concepts such as “telerehabilitation”, “e-rehabilitation”, “telemedicine”, “telecare”, “telehomecare” or “telehealth” (12-15). The concepts are often used interchangeably, and may be difficult to tell apart. We have chosen to use Lai et al.s (16) definition of telerehabilitation: “Telerehabilitation is the provision of distance support, assessment and intervention to individuals with disabilities via telecommunication, and is a subcomponent or the broader area of telemedicine.” (16).
The definition emphasises that telerehabilitation entails that health services may be offered at a distance, in particular to users in sparsely populated areas. Telerehabilitation (TR) is often used as a collective term and describes health services where traditional rehabilitation is used in combination with advanced technology, such as VC. Langberg et al. (17) divide TR into three categories: image based TR, sensor based TR and TR based on virtual technologies. TR may take place either through synchronous solutions (in real time), enabling direct contact between user and therapist, or asynchronous solutions (off line) with a “stand-in” – a virtual therapist (17).
TR may be used in the primary health care services without the involvement of the specialist health care services. TR may also be used within the specialist health care services, or between the specialist health care services and the primary health care services. The latter way of organising TR demands proper coordination between the two administrative levels in the health services. In order to find an adequate collective concept to cover both everyday rehabilitation and the use of VC technology, which we here consider a subcategory of traditional TR, we introduce the concept “tele-everyday- rehabilitation”. The concept is a combination of the words “tele” and “everyday rehabilitation”. The prefix “tele” shows that teletechnology is used to transfer information, e.g. by using video communication equipment in connection with treatment or transfer of information in general. “Everyday rehabilitation” entails a rehabilitation service in close collaboration and integration with the home care services (4), and covers early intensive and interdisciplinary rehabilitation in the home.
Tele-everyday-rehabilitation we thus define as a relatively intensive and short-term treatment method used to support the users’ resources in their own home, rather than having care personnel take over functions for the elderly person. Tele-everyday-rehabilitation also encompasses the technology used to reach users at a distance, as with video communication equipment which connects user(s) and therapist(s) through a secure Internet connection. In this context a secure Internet connection in Norway will entail using the service of Norsk Helsenett SF ( www.nhn.no) to transfer digital information.
Everyday rehabilitation in a municipality is traditionally performed by ergo therapists and physical therapists who collaborate closely with nurses or other health care personnel. The same ergo therapists and physical therapists will generally follow up one user, but the people from the home health services who go through the treatment programme with the user will frequently change. Even if such persons have proper knowledge of everyday rehabilitation they do depend on supervision and follow-up from an ergo therapist and physical therapist in order to quality assure that the exercises are done correctly. With a tele-everyday-rehabilitation programme it is possible to give supervision at a distance by using synchronous VC technology.
Figure 1 shows how we have chosen to place telemedicine, telerehabilitation and tele-everyday-rehabilitation along the dimensions of treatment intensity (high intensity vs low intensity) and the dimension of treatment duration (short-term vs long-term). In addition we distinguish between context: the specialist health services (hospital) vs primary health services. In the context of primary health services the tele-everyday-rehabilitation will normally take place in the home of the individual user, while traditional tele-everyday-rehabilitation may also take place in institutions. Traditional telerehabilitation will frequently be of longer duration (months or years) and have a lower treatment intensity compared to what we have chosen to call tele-everyday-rehabilitation.
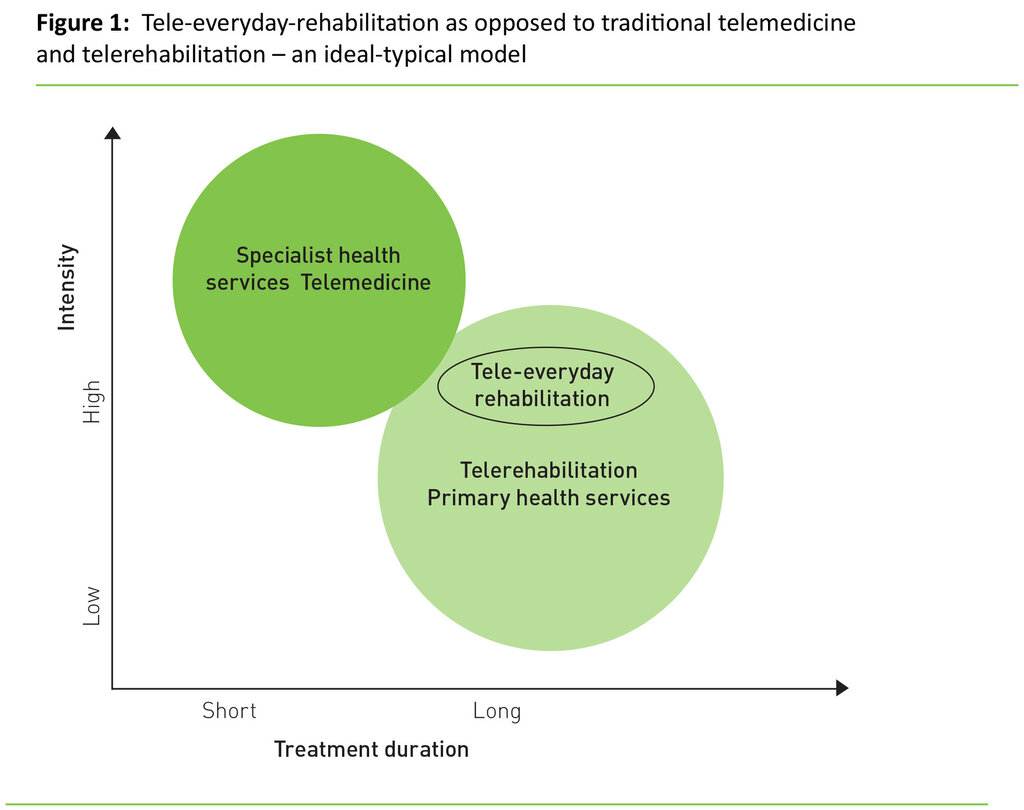
In the upper left hand corner (Figure 1) one finds the context in which telemedicine is traditionally offered. Telemedicine has its origin in the specialist health services and medicine, and may encompass areas such as telepathology, telesurgery, teletherapy and a series of other specialties. Compared to health services which traditionally are offered by the primary health services, ideal-typical features of using telemedicine and treatment in hospital is that the patient’s treatment is intensive and of relatively short duration (18). The treatment in the primary health services, in particular of the group of elderly with multiple diagnoses, is generally of relatively long duration and offered with fairly low intensity (4).
Tele-everyday-rehabilitation is thus distinct from traditional rehabilitation in the primary health services in that the treatment is fairly intensive, entailing physical training and training in everyday activities under supervision, and that the programme is frequently short-term (4-10 weeks). The overlapping of the circles suggests that the development and emphasis of the administration of regional health authorities and municipalities go in the direction of more coordination and emphasis on a holistic patient trajectory between the health services (19). Using a variety of types of technologies may be one of several ways of ensuring an improved rehabilitation trajectory for the patient (20).
Use of VC and telemedicine solutions
VC is a priority in the Norwegian Directorate of Health’s plan on electronic collaboration and has for many years been used as a tool in the expansion of telemedicine (20). VC can potentially strengthen collaboration and accessibility within the health services through offering individual health services independent of distance, such as follow-up and collaboration around rehabilitation of patients. The use of telemedical services in Norway is low in comparison with the number of face-to-face consultations (20). In Norway video communication has not yet become an established way of working in the specialist health services. The status of use and extent of this type of rehabilitation services in the primary health services is not known. There is, however, some trial project activity, a. o. in Arendal and Kristiansand, looking into how mobile units (PDA=personal digital assistant) may support the everyday rehabilitation effort (21). VC technology does not, however, enter into the latter trial. Everyday rehabilitation in general, that is, without VC technology, is more common (4). According to Meld. St. 26 (2014-2015) there were 100 municipalities in Norway in 2015 with practical experience with everyday rehabilitation, and more had plans of starting up (8).
Method
As mentioned in the introduction, scoping review has been chosen as research design for this study. According to Arksey and O’Malley (10) a series of arguments favour scoping review. We have taken our point of departure in one of several justifications for using scoping review as method: “To summarize and disseminate research findings: this kind of scoping study might describe in more detail the findings and range of research in particular areas of study, thereby providing a mechanism for summarizing and disseminating research findings to policy makers, practitioners and consumers who might otherwise lack time or resources to undertake such work themselves.” (10)
Like systematic literature studies, scoping review studies entail that the researcher systematically approaches and reviews available literature on a subject. A literature study thus entails gaining an overview of the relevant literature in the field in question. A review of the literature may give a basis for further investigations of the phenomenon, but will here be used for planning trial projects in municipalities in connection with tele-everyday-rehabilitation. Our “scoping” is a literature study that is a less extensive and explorative mapping of the research literature in the chosen field. Knowledge from our literature study shall be used to prepare for the expected challenges related to trying out this kind of technology in the municipalities. This entails a belief that a municipality may prepare for a certain type of challenges.
We have performed a systematic literature search. Search words and inclusion and exclusion criteria were defined in advance. We searched the databases CINAHL, Science Direct and PubMed. The search was performed on March 12 2015. The search phrase used was “reablement OR everyday rehabilitation OR active service model OR restorative home support AND telerehabilitation OR telecare OR telemedicine OR telehealth”.
The inclusion criteria were older users (patients) aged 65 +, living at home, competent to consent to participation, and had used video communication. Some of the included studies have a mixed user group, but include users over 65 years of age.
We included only original articles published in English in journals with peer review during the period 2004 to 2015. The search yielded a total 1060 hits. CINAHL yielded 632 hits, PubMed 60 hits, while Science Direct yielded 368 hits. After having selected overlapping included articles, 174 articles were selected based on the content of the abstracts. Of these 153 articles were excluded as they did not fulfil the inclusion criteria. The remaining 11 articles were included in our sample. We accessed all full-text versions of the articles. The analysis followed a multiple step procedure: 1) The articles were first read by first author, 2) first author worked out categories based on what we wanted to know, 3) the articles were uploaded to Nvivo for further analyses, and 4) based on the coding of the content in the articles, first author made summaries which have been transferred to three tables in the result section:
- A table showing the result of research based on the user perspective
- A table based on the perspective of health personnel
- A table based on the perspective of organisations
Second author has contributed with practical experience of everyday rehabilitation and has read the selected articles and participated in all phases of the writing process.
User experiences
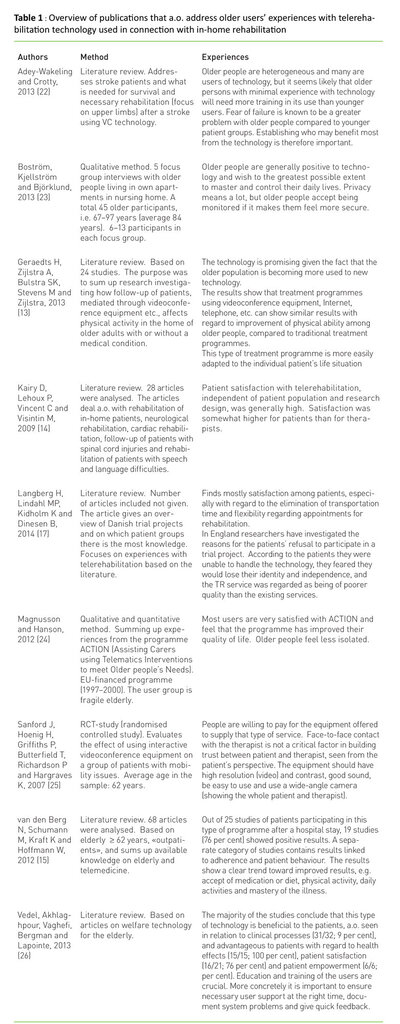
Table 1 gives an overview of summed up knowledge where the point of departure is older users’ experience with video communication equipment or similar technology used in connection with telerehabilitation.
Table 1 shows that users to a great extent are satisfied with TR. However, care should be taken with this kind of study as several have excluded users with cognitive failure, or as van den Berg et al. (15) points out:
«Older patients have a higher prevalence of comorbidities including physical or cognitive impairments that influence the ability to use technical devices or communicate by telephone or video-conference. However, in 26 of 68 included studies, patients with such characteristic comorbidities and limitations were excluded.» (15)
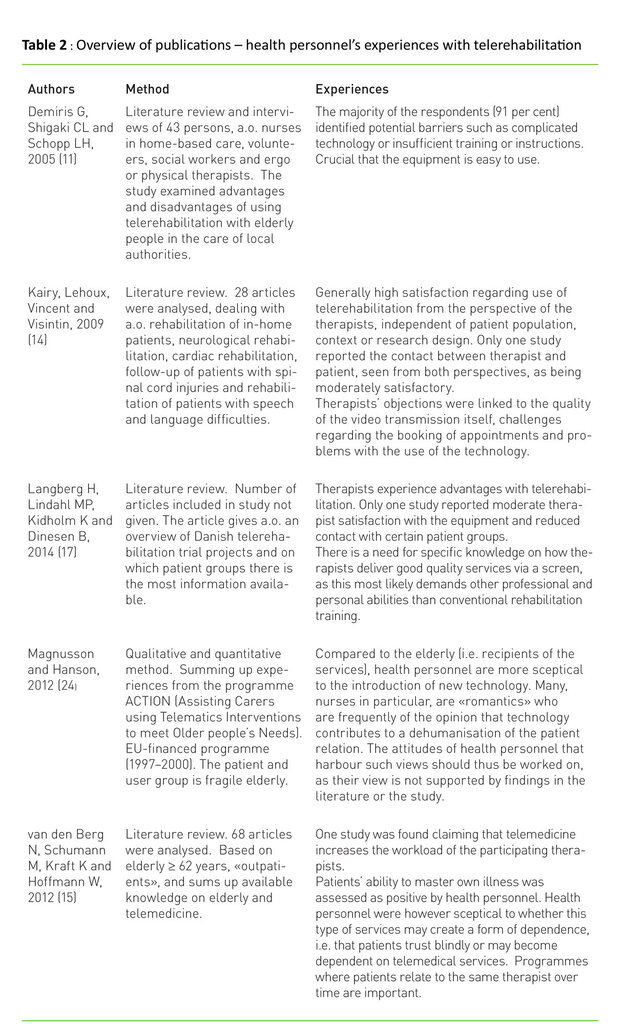
The experiences of health personnel
Professionals’ accept of such technology is in this type of technology project often put to the test due to a lack of knowledge, general scepticism or a lack of clinical basis and justification for the change. Several studies recommend attention to training and collaboration with health personnel and users. In table 2 we have summed up some of the findings based on the literature in question.
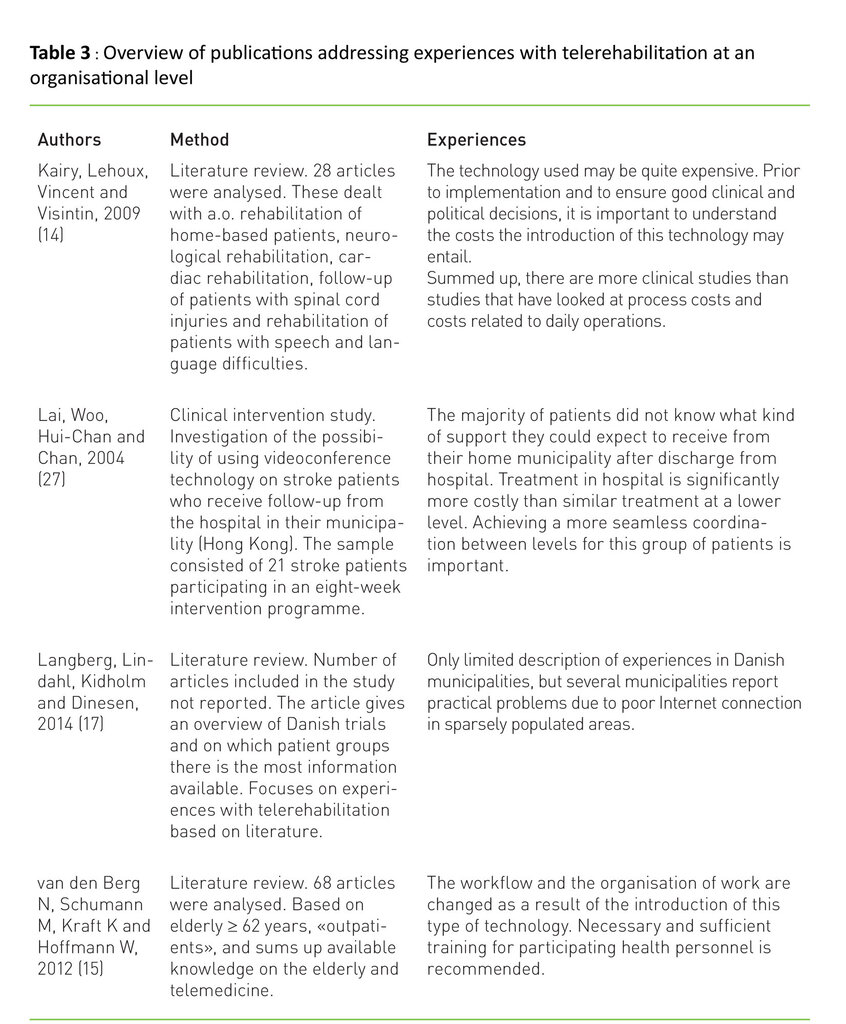
Experiences of the health organisations in the primary health services
Earlier research shows that the implementation of TR and/or telemedicine may constitute an organisational challenge. The challenge is particularly great in the transition from being a trial project to becoming an integrated part of the health services (20). In table 3 we show some findings where the organisational implications of telerehabilitation have been studied.
Discussion
The major part of the research we found is based on studies from the USA. Due to dissimilarities between countries, such as differences in national cultures (28), differences in laws and regulations regarding the financing of telerehabilitation services (29), and differences in the organisation of primary health services (30), we are of the opinion that one must be critical to whether such knowledge is relevant and transferable to a Norwegian health services context. We cannot wholly exclude the possibility that we may have missed studies that should have been included in our scoping review.
Research question 1 aimed at surveying experiences users have with VC technology in rehabilitation and/or everyday rehabilitation contexts. Our scoping review has shown that older users (aged 65+) are mainly satisfied with home-based health services where VC technology has been used. So TR may constitute an alternative or supplement to traditional rehabilitation (15,21,23,24). Users must, however, receive the necessary help with handling this technology, for instance with the in-home trainer taking the responsibility for this.
In Norway many elderly are in good health, and elderly Norwegians express a wish to remain in their homes as long as possible and to preserve independence and personal mastery in spite of illness and suffering (8). The Norwegian population is also quite advanced in the use of technology – many elderly are used to teleservices (bank services, tax services) and handle computers, tablets and smart phones. We therefore have reason to believe that elderly Norwegians are well motivated and at the outset positive to using VC technology. Local trial projects in Møre and Romsdal show great success with introducing Skype in nursing homes to improve contact between residents and family. Krøvel (31) found that the frail elderly enjoy Skype the most; they can communicate with family in spite of language barriers and cognitive challenges (31).
To succeed with this kind of treatment programme, seen from a user perspective, literature points out that user training is necessary, the equipment should be easy to use, and sound, contrast and screen resolution should be adapted to the elderly user’s needs (see table 1). With regard to the latter point, research gives no concrete recommendations when it comes to VC equipment, Internet speed etc. The reason may be that this type of technology changes fast, and that the types of equipment, set-up, configuration, etc. are relatively varied and extensive. This is clear from local trial projects; the challenges with Internet technology and digital systems create resistance in the users (32). Experience shows that technology should be stress-tested in other places than with the end user, such as in a trial apartment (32).
The other research question we wanted to know about was the health personnel’s perspective. Summed up research (se table 2) shows that health personnel is relatively satisfied with telerehabilitation. Here as well there will be a need for necessary training given before the organisation establishes such services. From an employer perspective it should be taken into consideration that not everyone will be positive to this type of services at the outset. In the research such scepticism is attributed to a. o. that the change may entail a redirection of the flow of work, change in the organisation of the work, fear of a weakening of the relation and trust between user and therapist, and a feeling of increased work-burden as a result of the changes (15,24). Paradoxically, older users rarely experience weakened trust as a problem in this context (15,23). That the older user has a designated and/or the same therapist over time, seems to be more important for the user and therapist relation than whether the encounter is physical or at a distance through VC (15).
Our third research question started from the experiences of organisations that have started using TR. The results from the organisations’ perspective are summed up in table 3. We found relatively few studies with this perspective. The existing studies show that this type of e-health service does not necessarily lead to a reduction in costs (34). Kairy et al. (14) point out that the technology used can be quite expensive. Prior to implementation, and in order to ensure good clinical and political decisions, it is important to understand what an introduction of telerehabilitation services may entail in the way of costs (14). There are, however, some uncertainties attached to this. Due to the complexity of the issue and a series of methodical challenges it is difficult and challenging to measure cost effectiveness in this context (35). However, several studies show that compared to treatment in hospital, it will be more cost effective to treat this type of patients locally, in the home or in an institution (15,35). Other challenges than the purely economical are addressed in other studies – e. g. problems with unstable Internet connections, increased expectations of training among the employees, and challenges linked to coordination and collaboration between various organisations (see table 3).
The purpose of the study was to assemble knowledge that may become useful in the planning and implementation of everyday rehabilitation supported by VC in a municipality. We have specifically chosen to focus on three perspectives, i.e. user, health personnel and organisations, which we find central to implementation of VC and everyday rehabilitation. In order to limit the study we have not commented on studies with a purely clinical focus, such as the effect of TR or similar treatment method on patients. We here refer the reader to earlier surveyed research that states that TR and/or similar treatment methods have fairly similar treatment results when these are compared with traditional rehabilitation (15,23,36).
Conclusion
The introduction of telerehabilitation will most likely make it easier to reach more users in their homes, especially in sparsely populated areas. Ergo and physical therapists can primarily supervise user and health personnel from the home health services at a distance through sound and image, and ensure that exercises are performed correctly.
The effect of the service will thus increase. By distinguishing between telerehabilitation and tele-everyday-rehabilitation analytically and definition-wise, we are of the opinion that it may be easier to compare research results as municipalities harvest experience with this type of health services. Our definition encompasses the technology, treatment method and idea foundation behind everyday rehabilitation, and should be used to distinguish tele-everyday-rehabilitation from traditional TR programmes.
This study may provide a basis for planning, implementing and trying out VC in everyday rehabilitation locally. At the same time the study also shows some of the challenges an introduction of this type of health services entails for users, health personnel and organisations. Thus tele-everyday-rehabilitation, and welfare technology in general, is no “quick fix” for solving the challenges in the primary health services.
Based on our findings we recommend that studies be performed in Norway with the aim of acquiring more knowledge of this kind of health services. The organisation perspective in particular is overlooked in research, and it would be interesting to assess cost – utility value in further studies. One could assess investment costs against possible gains in the form of increased personal mastery and quality for the user, and thus postponement of need for services. As there is a shortage of research in this area in Norway, we hope the funding authorities will make a priority of this in the future.
References
1. SSB. Statistisk sentralbyrå. Folkemengde, 1. januar 2015. Statistisk sentralbyrå, Oslo. 2015. Available from: https://www.ssb.no/befolkning/statistikker/folkemengde.
2. Helse- og omsorgsdepartementet. Innovasjon i omsorg (2011:11). Helse- og omsorgsdepartementet, Oslo. 2011.
3. Romøren TI. Den fjerde alderen : funksjonstap, familieomsorg og tjenestebruk hos mennesker over 80 år. Gyldendal Akademisk, Oslo. 2001.
4. Tuntland H, Ness NE. Hverdagsrehabilitering. 1. utg. Gyldendal Akademisk, Oslo. 2014.
5. Månsson M. Hemrehabilitering: vad, hur och för vem? : Fortbildning AB. 2007.
6. Glendinning C, Newbronner E. The effectiveness of home care reablement – developing the evidence base. Journal of Integrated Care 2008;16(4):32–9.
7. Gaugler JE, Zarit SH, Pearlin LI. Family involvement following institutionalization: Modeling nursing home visits over time. International Journal of Aging & Human Development 2003;57(2):91–117.
8. Meld. St. 26. Fremtidens primærhelsetjeneste – nærhet og helhet. Helse- og omsorgsdepartementet, Oslo. 2014–2015 (s. 168).
9. Kjellberg PK, Ibsen R, Kjellberg J. Fra pleje og omsorg til rehabilitering. Erfaringer fra Fredericia Kommune. 2011 Contract No.: DSI project 3106.
10. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology 2005;8(1):19–32.
11. Demiris G, Shigaki CL, Schopp LH. An evaluation framework for a rural home-based telerehabilitation network. Journal of Medical Systems 2005;29(6):595–603.
12. Ekeland AG, Bowes A, Flottorp S. Effectiveness of telemedicine: A systematic review of reviews. International Journal of Medical Informatics 2010;79(11):736–71.
13. Geraedts H, Zijlstra A, Bulstra SK, Stevens M, Zijlstra W. Effects of remote feedback in home-based physical activity interventions for older adults: a systematic review. Patient Educ Couns. 2013;91(1):14–24.
14. Kairy D, Lehoux P, Vincent C, Visintin M. A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disability & Rehabilitation 2009;31(6):427–47.
15. van den Berg N, Schumann M, Kraft K, Hoffmann W. Telemedicine and telecare for older patients – a systematic review. Maturitas 2012;73(2):94–114.
16. Lai JCK, Woo J, Hui E, Chan WM. Telerehabilitation – a new model for community-based stroke rehabilitation. Journal of telemedicine and telecare 2004;10(4):199–205.
17. Langberg H, Lindahl MP, Kidholm K, Dinesen B. Telerehabilitering. Ugeskr Læger 2014;176(10):944–7.
18. Grimsmo A. Veien frem til helhetlig pasientforløp, Norsk helsenett, Trondheim. 2012. Available from: http://www.nhn.no/samhandling/helhetlig-pasientforloep. (Downloaded 5. August 2013).
19. Grimsmo A, Kirchhoff R, Aarseth T. Samhandlingsreformen i Norge. Nordiske organisasjonsstudier. 2015;17(3):3–12.
20. Zanaboni P, Knarvik U, Wootton R. Adoption of routine telemedicine in Norway: the current picture. Global Health Action; vol. 7 (2014) incl. supplements. 2014.
21. Linander H, Asones EH. Hverdagsrehabilitering – Teknologistøtte. InnoMed, 2014.
22. Adey-Wakeling Z, Crotty M. Upper limb rehabilitation following stroke: current evidence and future perspectives. Aging Health 2013;9(6):629–47.
23. Boström M, Kjellström S, Björklund A. Older persons have ambivalent feelings about the use of monitoring technologies. Technology & Disability 2013;25(2):117–25.
24. Magnusson L, Hanson E. Partner-ship working: The key to the AT-technology transfer process of the ACTION service (Assisting Carers using Telematics Interventions to meet Older people’s Needs) in Sweden. Technology and Disability 2012;24:219–32.
25. Sanford J, Hoenig H, Griffiths P, Butterfield T, Richardson P, Hargraves K. A Comparison of televideo and traditional in-home rehabilitation in mobility im-paired older adults. Physical & Occupational Therapy In Geriatrics 2007;25(3):1–18.
26. Vedel I, Akhlaghpour S, Vaghefi I, Bergman H, Lapointe L. Health information technologies in geriatrics and gerontology: a mixed systematic review. Journal of the American Medical Informatics Association. JAMIA 2013;20(6):1109–19.
27. Lai JCK, Woo J, Hui-Chan E, Chan WM. Telerehabilitation – a new model for community-based stroke rehabilitation. Journal of telemedicine and telecare 2004;10(4):199–205.
28. Hofstede GH, Hofstede GJ. Culture and organizations – software of the mind. McGraw-Hill. 2005.
29. Calouro C, Mei KW, Gutierrez M. An analysis of State telehealth laws and regulations for occupational therapy and physical therapy. International Journal of Telerehabilitation. 2014;6(1).
30. Krasnik A, Paulsen B. Reforming primary health care. I: Magnussen J, Vrangbæk K, Saltman R (red.). Nordic health care systems: recent reforms and current policy challenges. McGraw-Hill International, Berkshire. 2009 (s. 233–54).
31. Krøvel SB. Innovasjon i omsorg. Utprøving av videokommunikasjonsteknologi i sykeheim. Beboer og pårørende i møte med en felles læringsarena (masteroppgave). Høgskulen i Volda. 2014.
32. Alnes RE, Berg H. Lokaliseringsteknologi – nytte og utfordringar : Ei undersøking om bruk av lokaliseringsteknologi for personer med kognitiv svikt. Fjordkonferansen, Loen. 18.–20. juni 2014.
33. Cudd PA, Magnusson L, Hanson E. Partnership working: The key to the AT-technology transfer process of the ACTION service (Assisting Carers using Telematics Interventions to meet Older people’s Needs) in Sweden. Technology & Disability 2012;24(3):219–32.
34. Hansen D, Golbeck AL, Noblitt V, Pinsonneault J, Christner J. Cost factors in implementing telemonitoring programs in rural home health agencies. Home Health-care Nurse 2011;29(6):375–82.
35. Vimarlund V. Economic analyses for ICT in elderly healthcare: questions and challenges. Health Informatics Journal 2005;11(4):309–21.
36. Sanford JA, Griffiths PC, Richardson P, Hargraves K, Butterfield T, Hoenig H. The effects of in-home rehabilitation on task self-efficacy in mobility-impaired adults: a randomized clinical trial. Journal of the American Geriatrics Society 2006;54(11):1641–8.






Comments