The pre-hospital path for patients admitted with suspected acute stroke
The remainder were referred by the out-of-hours primary healthcare service or their GP. These patients were younger than those admitted by ambulance.
Background: Time is of the essence in the event of a stroke, but still less than half of the patients arrive at hospital within four hours of the onset of symptoms. A possible explanation for this delay is that their first contact with the health service is via the out-of-hours primary healthcare service or their GP.
Objective: The objective of this study was to map the referral unit for patients with a suspected acute stroke prior to arriving at the A&E department at Oslo University Hospital, Ullevål. We also wanted to map whether the referral unit could be correlated with stroke diagnosis on discharge.
Method: A retrospective observation study identified all patients admitted with suspected stroke at the A&E department, Oslo University Hospital, Ullevål in 2018. We grouped patients according to the referral unit: ambulance, out-of-hours primary healthcare service, GP practice or direct admission. We compared the discharge diagnoses ‘stroke’ or ‘non-stroke’ according to the referral unit and age distribution using the chi-square test.
Results: A total of 1399 patients with suspected stroke were admitted, of whom 594 (42 per cent) received a stroke diagnosis. The median age was 72 years, and 52 per cent were women. Half of the patients were admitted directly by ambulance, a third via the out-of-hours primary healthcare service and 12 per cent via the GP practice. Significantly more patients admitted by ambulance (51 per cent) were discharged with a stroke diagnosis compared with patients from the out-of-hours primary care service (29 per cent) or a GP practice (40 per cent) respectively (chi-square p < 0.001). The patients who were admitted by ambulance were significantly older than those admitted via the out-of-hours primary healthcare service (72 years versus 65 years, p < 0.001).
Conclusion: Only half of the patients with symptoms of suspected stroke were admitted by ambulance. Patients admitted directly by ambulance were more often discharged with a stroke diagnosis. We need more knowledge about the reasons why the remaining patients were admitted via their GP or the out-of-hours primary healthcare service.
In Norway, approximately 12 000 patients annually have a stroke (1). Considerable progress has been made in hospital treatment and management particularly at hospitals where patients are met by a team of doctors and registered nurses (RNs) with special expertise in this field.
Time is of the essence in the event of a stroke, but still less than half of the patients arrive at hospital within four hours of the onset of symptoms (2).
Stroke patients have complex symptomatology and diffuse presentation, and consequently exhibit a complex clinical picture to their first point of contact. Therefore, rapid identification of the condition and immediate transport to hospital are essential. A good prognosis after a stroke depends on all phases of the treatment, as the time from the onset of symptoms to treatment determines the outcome (1).
The pre-hospital patient pathway involves many different healthcare professions. For RNs, identifying the symptoms of a stroke in both telephone consultations and when meeting the patient in person is crucial. The latter may take place in the ambulance, at the out-of-hours primary healthcare service, at the GP practice or on a home visit.
There may be delays at all stages of the pre-hospital path. Earlier research shows that pre-hospital factors account for half of all the delays (7).
Another study showed that six out of ten patients who contacted the primary healthcare service were asked to attend the GP practice or the out-of-hours primary healthcare service, leading to unnecessary loss of time (5). Therefore, knowledge of the patient pathway up to hospital admission is important for improving treatment for all patients with acute stroke.
Objective of the study
The objective of this study was to map the referral unit for patients with suspected acute stroke prior to arriving at the A&E department, Oslo University Hospital, Ullevål.
Method
We identified all the patients admitted with suspected stroke to the A&E department, Oslo University Hospital, Ullevål, in 2018. The patients were identified retrospectively by extracting data from the electronic patient record. We manually registered age, gender, referral unit, reason for admission and main diagnosis on discharge.
We defined the following registered admission reasons as suspected stroke: ‘thrombolysis’, ‘stroke’, ‘stroke/apoplexy/cerebral insult’, ‘TIA’, ‘dizziness assessed by neurologist’, ‘diplopia’, ‘numbness’, ‘aphasia/dysarthria’, and ‘hemiparesis’.
We also registered the patient’s discharge diagnosis/diagnoses according to the ICD-10 system, an international classification of diseases. A stroke-related discharge diagnosis was defined as G45.9, unspecified transient cerebral ischemic attack, I61, nontraumatic intracerebral haemorrhage, and I63, unspecified cerebral infarction. We did not include I64, stroke, not specified as haemorrhage or infarction, in our study.
We registered the referral unit in one of the following categories: ambulance, out-of-hours primary healthcare service, GP, other hospital or attendance at the A&E department. Age and gender were registered for all patients, but supplementary diagnoses or treatment during the hospital stay were not recorded.
Patients admitted with other diagnoses who had a stroke during their hospital stay were not included in the study.
Statistics
Age is presented as median values with a lower and upper quartile. Category data are given in absolute figures and percentage values. We examined the differences in discharge diagnoses at the registered referral units using a chi-square test. The difference between the various age groups was analysed using ANOVA.
In addition, we sorted age groups into quartiles and used the chi-square test to analyse the differences between the registered referral units in terms of age quartiles.
Finally, we compared the discharge diagnoses of patients in the upper age quartile with patients in the lower age quartile, again by using the chi-square test. P-value < 0.05 was determined to be statistically significant. We performed statistical analyses using IBM SPSS Statistics, version 25.
Ethics
The study was approved by the Regional Committees for Medical and Health Research Ethics (REC) as part of the research programme Dispatch Norwegian Acute Stroke Prehospital Project (DispatchNASPP) (case number 2018/1909). We also notified the local data protection officer (case number 18/25297).
We applied for exemption from the consent requirement, which meant that the information could be obtained without the hindrance of the duty of confidentiality. The study is simply a mapping of what has happened and has no impact on the patients’ course of treatment.
Results
In 2018, a total of 1399 patients were admitted with suspected acute stroke. Of these, 594 (42 per cent) were discharged with a stroke-related diagnosis. The median age for those with acute stroke was 72 years (59–83), and 52 per cent were women.
Admission categories
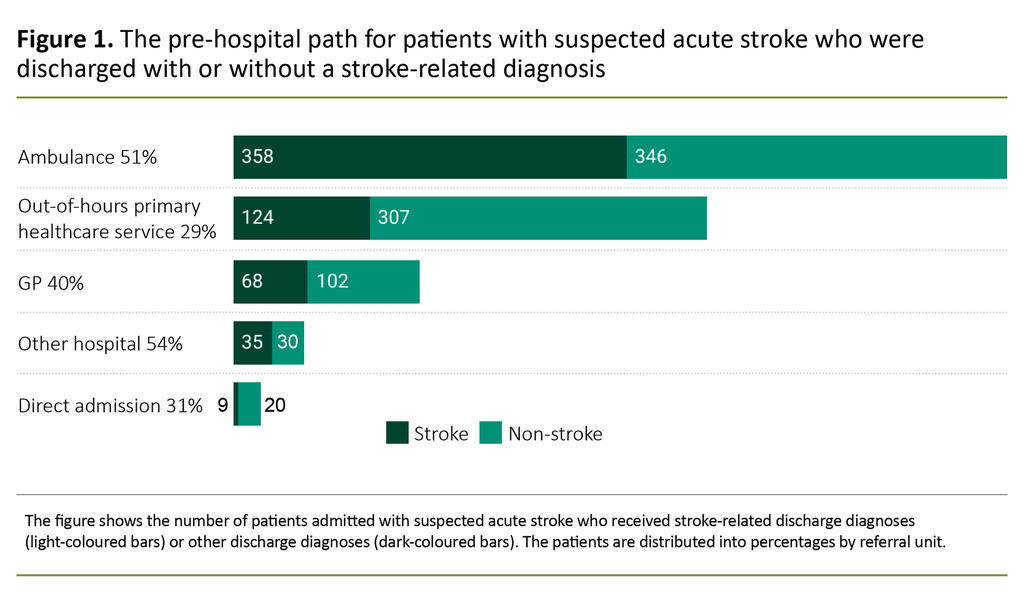
Figure 1 shows the pre-hospital path for all patients, distributed by the discharge diagnosis ‘stroke’ or ‘non stroke’. Approximately half of the patients were admitted directly by ambulance. Of these, 358 out of 704 (51 per cent) were discharged with a stroke-related diagnosis. In a third of the cases, the out-of-hours primary healthcare service was registered as the referral unit, and 124 out of 431 (29 per cent) of these patients were discharged with a stroke-related diagnosis.
The corresponding figure for GPs was 68 out of 170 (40 per cent). The percentage with a stroke discharge diagnosis showed a statistically significant difference between those with and those without a stroke-related diagnosis (p < 0.001). A small percentage was registered as coming from another hospital: 65 (5 per cent), or as attending the A&E department directly: 29 (2 per cent).
Age
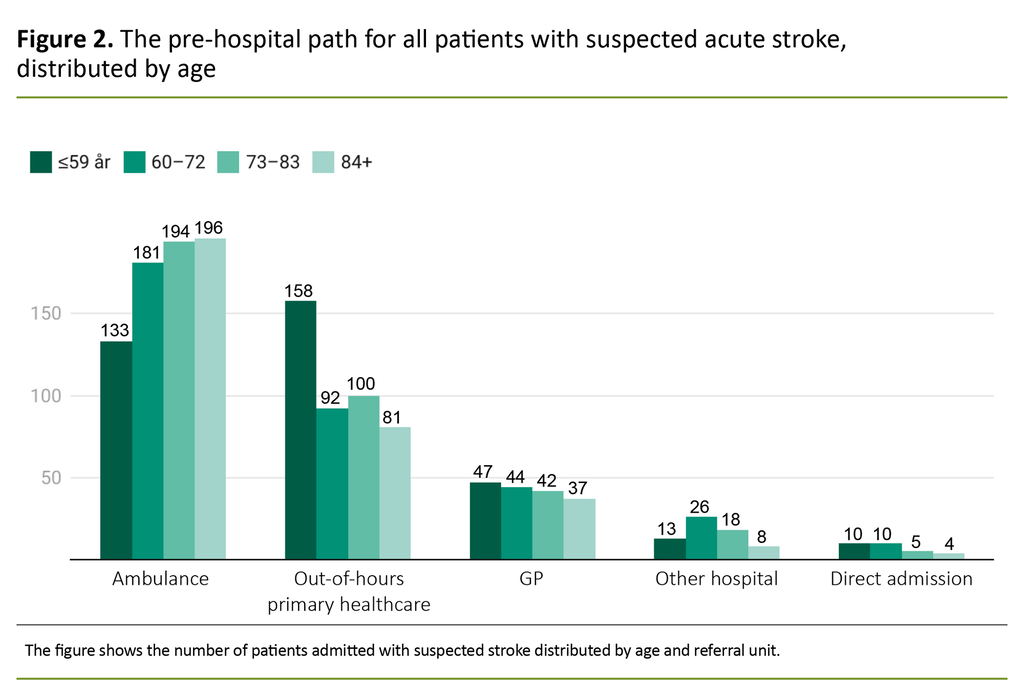
Figure 2 shows the registered referral body distributed by age quartiles. The patients arriving by ambulance were significantly older than those who arrived via the out-of-hours primary healthcare service (72 years versus 65 years, p < 0.001). The youngest patients (≤ 59 years) were admitted via the out-of-hours primary healthcare service or GP practice significantly more often than older patients (> 60 years, p < 0.001).
Significantly fewer patients in the youngest age quartile were discharged with a stroke-related diagnosis compared with the three oldest quartiles: 96 out of 361 (27 per cent) versus 498 out of 1038 (48 per cent, p < 0.001).
Distribution of non-stroke diagnoses
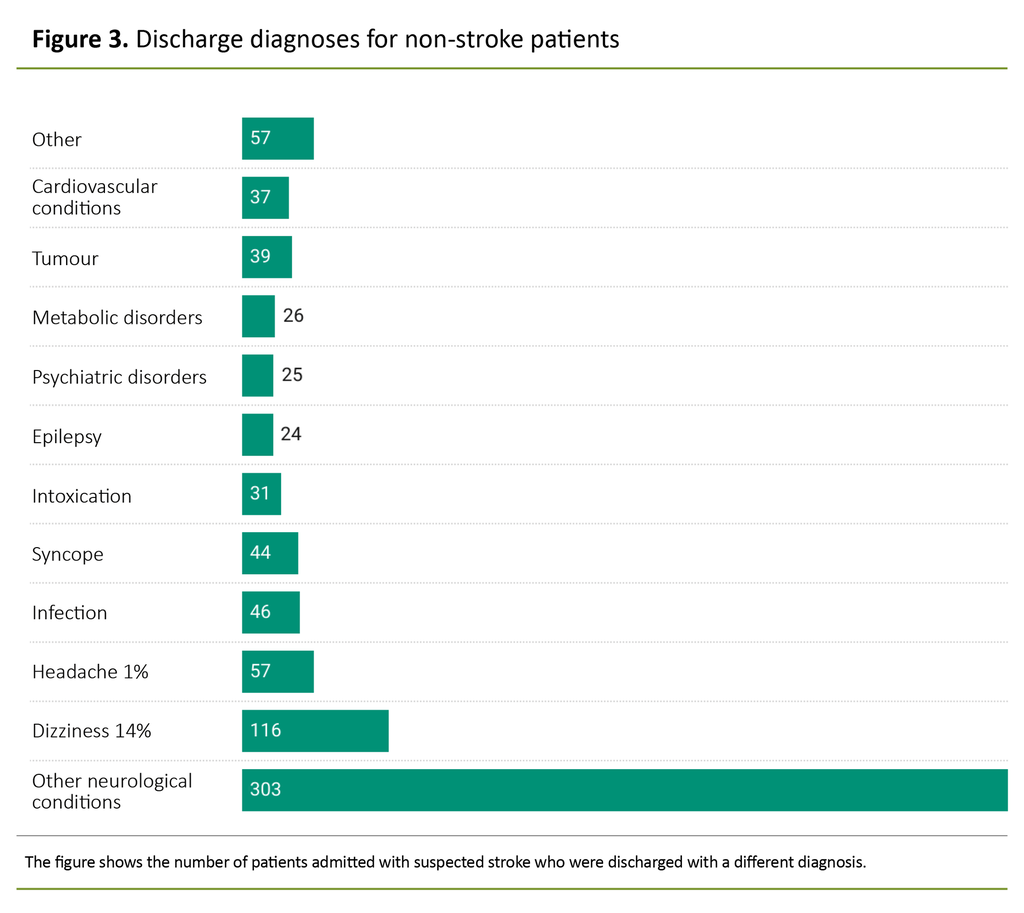
Of the 1399 patients admitted with suspected stroke, 805 (57 per cent) were discharged with a different ICD-10 diagnosis code. The category ‘other neurological disorders’ included 54 different diagnoses (ICD-10), such as visual disorders, diplopia and neck pain.
The category ‘Other’ covers diagnoses relating to other organ systems such as fractures, anaemia, kidney disease, chronic obstructive pulmonary disease, ileus, stomach pain, burns and nausea (Figure 3).
Discussion
Only half of all the patients admitted to Oslo University Hospital with suspected stroke in 2018 were directly admitted by ambulance. The remaining patients came from the out-of-hours primary healthcare service, a GP practice or another hospital, or they came directly to the A&E department.
Age differences
The findings of this study show that fewer patients in the youngest age quartile were discharged with a stroke-related diagnosis compared with the oldest quartile. The patients admitted by ambulance were significantly older and more often received a stroke-related diagnosis than those arriving via the out-of-hours primary healthcare service or a GP practice. The reason that younger patients contacted the out-of-hours service first may be that they had milder or atypical symptoms, so that conditions other than stroke were assessed as more likely (5, 6).
Another reason may be that doctors have a lower threshold for admitting younger patients if stroke is suspected because the consequences of misdiagnosis may result in the patient having to live with long-term effects for the rest of their lives.
The reason why the ambulance service is more able to recognise stroke-related symptoms may be that they are most likely to be contacted when the patient is showing obvious symptoms of a stroke. It is important to note that, in this material, the clinical assessment of the patient is performed by the ambulance crew, making this the only category in the pre-hospital pathway where the patient is not assessed by a doctor.
Pre-hospital delay
Doggen et al. showed that almost half of the stroke patients contacted the out-of-hours primary healthcare service or a GP practice prior to arriving at the stroke unit, and half of the patients who had contacted their GP were transported to hospital by ambulance. The remainder used private transportation. The average time from the onset of symptoms to arrival at the A&E department was 240 minutes, and half of the patients waited more than four hours before seeking medical advice (6).
A Norwegian study showed that patients who contacted an ordinary GP practice had less severe neurological symptoms and a greater delay in admission than patients who contacted the Emergency Medical Communications Centre (AMK) (5, 6).
If the time from the patient’s first contact with the health service until their arrival in hospital is prolonged, this may mean that fewer patients receive reperfusion therapy. Data from the Norwegian Stroke Registry shows that in 2018, only 45 per cent of patients with suspected stroke were admitted to Ullevål Hospital within four hours of symptom onset (2).
The results indicate that there is a need to provide the public with more information in the form of new campaigns that can boost knowledge of risk factors in the population and show the importance of contacting the AMK when stroke is suspected (7–9).
Need for pre-hospital competence
Pre-hospital competence is vital for all professional groups working in the various parts of the health service in non-hospital settings, whether home-based nursing care, GP practices, local emergency medical communication centres, the out-of-hours primary healthcare service, AMK, ambulance, air ambulance or the A&E department.
The key role of RNs and ambulance personnel involves being able to suspect and recognise stroke on the basis of the patient’s symptoms. Furthermore, the interdisciplinary cooperation vis-à-vis the patient must also ensure swift and correct treatment and care.
Hospital referral via the out-of-hours primary healthcare services and GP practices may entail a delay for patients with suspected stroke (6). It is crucial that the general public has more knowledge about stroke symptoms and the need to call the emergency number 113. Moreover, staff in medical emergency services (AMK and local emergency medical communication centres), the ambulance service, RNs and doctors in the primary healthcare service must be better equipped to identify patients with suspected stroke (10).
Conducting a high-quality pre-hospital clinical assessment would be challenging because it requires pre-hospital personnel to have excellent assessment skills, and there are few screening tools available (10).
A study from Oslo University Hospital has led to competence enhancement among ambulance personnel as they have adopted the same screening tool as doctors in the stroke unit for patients with suspected stroke, namely the National Institutes of Health Stroke Scale (NIHSS) (11).
This scale has been developed as a mobile app for clinical decision support, and it functions as both a communication tool and electronic documentation. The results of the study were published in 2022. A national plan should be devised for the skills development and training of pre-hospital personnel in identifying a stroke, including recognition of the symptoms and the use of NIHSS, for example.
The challenge is that the symptom profile can resemble stroke but might have a different cause – in other words, ‘a stroke chameleon’, i.e. a condition assessed as something other than stroke, where stroke is thus overlooked (12).
A final diagnosis must be made after advanced in-hospital diagnostics, something that is impossible to achieve with the currently available pre-hospital tools. This means that in the case of a highly complex condition such as stroke, we can assume that patients admitted with suspected stroke will often be discharged with a different diagnosis. Hospitals must therefore take into account that a number of the patients admitted will not receive a stroke diagnosis, so-called overtriage (12).
In other words, it is not merely expertise in the form of clinical understanding that is necessary but also access to advanced medical equipment. Early pre-hospital identification of stroke and the correct level of triage may result in more patients receiving acute treatment.
Symptoms of stroke may be non-specific and assessing them is complex, so good communication and the use of a common language between pre-hospital services and stroke unit doctors are essential. We need to improve pre-hospital diagnostics of acute stroke so that in the future, more patients can be treated within the critical time window (9).
Strengths and weaknesses of the study
A strength of this study is that it includes a complete dataset of patients admitted with suspected stroke and assessed at an A&E department with a high volume of patients. The quality indicators are the same as in the Norwegian Stroke Registry. The generalisability of the results to other parts of Norway depends on several factors, such as distance to and accessibility of a hospital, out-of-hours primary healthcare service and GP practice.
A weakness of the study is the lack of clinical data including risk factors, neurological examination and the etiology of the stroke. Another weakness is that our data material is obtained from only one data source. We obtained data about the referral unit by extracting data registered by healthcare personnel in the electronic patient record.
We were unable to check or verify other sources such as patient records in the primary health service, AMK’s computer assisted dispatch system, ambulance records or direct access to hospital records.
In addition, it would have been useful if the time from symptom debut to admission had been registered for the different categories, particularly for the quality indicator ‘four hours from symptom debut to hospital admission’. Our material also fails to describe whether patients admitted via the out-of-hours service or the GP practice had contacted the AMK first, or if they were transported to the GP practice by ambulance first for a more detailed assessment prior to hospital admission.
Conclusion
A large percentage of patients admitted to hospital with suspected stroke do not arrive by ambulance. Those who arrive by ambulance were significantly older than patients who arrived via the out-of-hours primary healthcare service. Fewer patients in the youngest age quartile were discharged with a stroke-related diagnosis compared with the oldest quartile.
It is important to strengthen competence in pre-hospital services, including the home-based nursing service, in order to ensure direct admission to hospital for diagnostics and acute treatment.
The authors declare no conflicts of interest.
References
1. Ormstad SS, Lund UH, Chudasama KK, Frønsdal KB, Hov MR, Ormberg I, Hafstad E, et al. Prehospital CT for tidlig diagnostikk og behandling ved mistanke om hjerneslag eller alvorlig hodeskader. Oslo: Folkehelseinstituttet; 2019. Rapport nr.: 978-82-8406-005-7. Available at: https://www.fhi.no/publ/2019/prehospital-ct-for-tidlig-diagnostikk-og-behandling-ved-mistanke-om-hjernes/ (downloaded 20.12.2021).
2. Fjærtoft H, Skogseth-Stephani R, Indredavik B, Bjerkvik TF, Varmdal T, Norsk hjerneslagsregister, St. Olavs hospital. Norsk hjerneslagsregister. Årsrapport 2019. Med plan for forbedringstiltak. Trondheim: St. Olavs hospital; 2019. Available at: https://www.kvalitetsregistre.no/sites/default/files/1_arsrapport_2019_norsk_hjerneslagregister_justert_21.10.2020.pdf (downloaded 01.11.2021).
3. Fjærtoft H, Phan A, Indredavik B, Norsk hjerneslagregister, St. Olavs hospital. Den nasjonale informasjonskampanjen om hjerneslag «Prate, smile, løfte». Trondheim: St. Olavs hospital; 2018.
4. Saver JL, Smith EE, Fonarow GC, Reeves MJ, Zhao X, Olson DM, et al. The «golden hour» and acute brain ischemia. Stroke. 2010;41(7):1431–9. DOI: 10.1161/STROKEAHA.110.583815
5. Faiz KW, Sundseth A, Thommessen B, Rønning OM. Prehospitalt forløp ved akutt hjerneslag. Tidsskrift for Den norske legeforening. 2017;137:798. DOI: 10.4045/tidsskr.16.0512
6. Doggen CJ, Zwerink M, Droste HM, Brouwers PJ, van Houwelingen GK, van Eenennaam FL, et al. Prehospital paths and hospital arrival time of patients with acute coronary syndrome or stroke, a prospective observational study. BMC Emergency Medicine. 2016;16(1):1–10. DOI: 10.1186/s12873-015-0065-y
7. Faiz KW, Sundseth A, Thommessen B, Rønning OM. Prehospital delay in acute stroke and TIA. Emergency Medicine Journal. EMJ. 2013;30(8):669–74. DOI: 10.1136/emermed-2012-201543
8. Wang R, Wang Z, Yang D, Wang J, Gou C, Zhang Y, et al. Early hospital arrival after acute ischemic stroke is associated with family members' knowledge about stroke. Front Neurol. 2021;12:652321. DOI: 10.3389/fneur.2021.652321
9. Ruiz RG, Fernández JS, Ruiz RMG, Bermejo MR, Arias AA, Saucedo PDS, et al. Response to symptoms and prehospital delay in stroke patients. Is it time to reconsider stroke awareness campaigns? J Stroke Cerebrovasc Dis. 2017;27(3). DOI: 10.1016/j.jstrokecerebrovasdis.2017.09.036
10. Brandler ES, Sharma M, McCullough F, Ben-Eli D, Kaufman B, Khandelwal P, et al. Prehospital stroke identification: factors associated with diagnostic accuracy. Journal of Stroke and Cerebrovascular Diseases. 2015;24(9):2161–6. DOI: 10.1016/j.jstrokecerebrovasdis.2015.06.004
11. Guterud MM, Bugge HF, Bache KCG, Braarud A-C, Eriksen E, Fremstad KO, et al. Paramedic Norwegian Acute Stroke Prehospital Project (ParaNASPP) study protocol: a stepped wedge randomised trial of stroke screening using the National Institutes of Health Stroke Scale in the ambulance. Trials. 2022;23(1):113. DOI: 10.1186/s13063-022-06006-4
12. Faiz K, Rand K, Barra M. Fremtidens hjerneslagdiagnostikk og hjerneslagimitatorer. Tidsskrift for Den norske legeforening. 2018;138(12). DOI: 10.4045/tidsskr.18.010






Comments