Testing of the SVIP (Strengthened supervision during clinical practice in nursing education) model in clinical practice in mental health nursing – a qualitative study
The supervision model was tested in this field for the first time. The lecturer provided guidance for the practice supervisors.
Background: In recent years, there has been a focus on improving the quality of clinical practice, which constitutes 50 per cent of the bachelor’s degree programme in nursing. Research on different supervision models is vital to ensure best practice. This study examines how nursing students and practice supervisors perceive the SVIP (Strengthened supervision during clinical practice in nursing education) model in clinical practice in mental health nursing. To the best of our knowledge, the SVIP model has not been tested previously in this field.
Objective: The objective of the study was to examine how nursing students and practice supervisors perceive the SVIP model in clinical practice in mental health nursing.
Method: The study applied a hermeneutic descriptive design. The data were collected through seven focus group interviews of nursing students and practice supervisors. We carried out a qualitative content analysis.
Results: Three main themes emerged in the analysis: 1) New roles in practice supervision and assessment, 2) The practice supervisor’s competence, and 3) Organisation and framework factors.
Conclusion: The study shows that strengthening the supervision skills of practice supervisors is important for nursing students’ learning. In order to develop and enhance the quality of clinical practice, it may be necessary to change roles that have remained static for years. A binding, close collaboration between the field of practice and the educational institutions is essential for promoting the learning processes of nursing students.
Introduction
Background
In Norway, the bachelor’s degree programme in nursing is regulated by national guidelines (1) based on an EC directive requiring 50 per cent of nursing education to consist of clinical practice (2). No clear requirements are set as to how to safeguard the quality of practice.
Internationally, there are major differences in the implementation of clinical practice, and different models are applied (3). In Norway, requirements vary in respect of the competence of both the educational institution’s academic staff and the registered nurses (RNs) who supervise nursing students in clinical practice.
The Ministry of Education and Research commissioned Universities Norway (UHR) to carry out a project on the quality of clinical practice (the clinical practice project) in the period 2013–2015. Following this project (4), several educational institutions that train nurses have tested new supervision models in clinical practice (5, 6).
The SVIP model (7) is one of several new models that have been tested (8, 9). It was tested for the first time at the former Gjøvik University College in 2008 (7, 8). The model partly evolved from guidelines in the Quality Reform in which factors such as the students’ learning environment and strengthened cooperation between educational institutions and clinical practice were emphasised, as indicated in Report No. 27 to the Storting (2000–2001) (30).
While the educational institutions have formal responsibility, the practice supervisor has professional responsibility for supervising and assessing students, based on the learning outcomes. The objective of the SVIP model is to strengthen practice supervisors’ competence. Currently, practice supervisors are not required to possess formal qualifications in supervision.
One of the suggestions in the clinical practice project was to develop a national study programme for practice supervisors via reciprocal cooperation between the placement provider and the educational institution. The Ministry of Education and Research is attempting to establish a standard whereby practice supervisors are required to have formal qualifications in supervision (10).
Previous research
Research shows that good quality clinical practice builds on a complex interplay of various factors. A reciprocal, binding cooperation between the placement provider and the educational institution is necessary to achieve quality (7, 11).
Dyar et al. (12) state that active participation, the competence of practice supervisors and their motivation are important elements of a good learning environment. O’Brien et al. (3) found that students sharpen their learning focus when they are actively involved in the various tasks of the department.
The practice supervisor’s competence is essential to safeguard the nursing student’s learning focus. A study shows that practice supervisors need continuous in-service training to enhance the quality of their own clinical supervision of nursing students (13). A closer and well-defined cooperation between the placement provider and the university was a prerequisite for effective supervision in clinical practice, and also resulted in practice supervisors wishing to improve their competence.
Practice supervisors move between different roles. They alternate from being responsible for patient treatment to being responsible for supervising nursing students (3). Stenfors-Hayes et al. (14) found that in their role as practice supervisors, RNs were eager to develop their clinical skills and act as a role model for the students. The clarification of role expectations and responsibilities is a key factor in the supervision.
A Finnish study (15) shows that practice supervisors who are part of a supervision team dealt well with the various challenges they faced. They benefitted from contact with each other and became more confident and more skilled in supervising the students.
Research shows that it is vital that practice supervisors are prepared and motivated for their role in making students responsible for their own learning (16, 17). Moreover, a good supervisor-student relationship is essential for ensuring that the student has the best possible outcome from the clinical placement (18).
Traditional clinical practice model versus the SVIP model
The traditional supervision model in nursing education in Norway involves a nursing student, a practice supervisor and a lecturer. They meet three times throughout the eight to ten-week placement. The nursing student follows the shifts of the practice supervisor and participates in the daily work of the placement provider during this period. This model has been used in Norway for many years, and the traditional description of the roles of the nursing student, the lecturer and the practice supervisor has changed very little (19).
However, Chapter 8, section 23 of the national curriculum regulations for nursing education (1) emphasises the following: The educational institution should offer training in supervision and the parties involved must collaborate on a plan to implement this.
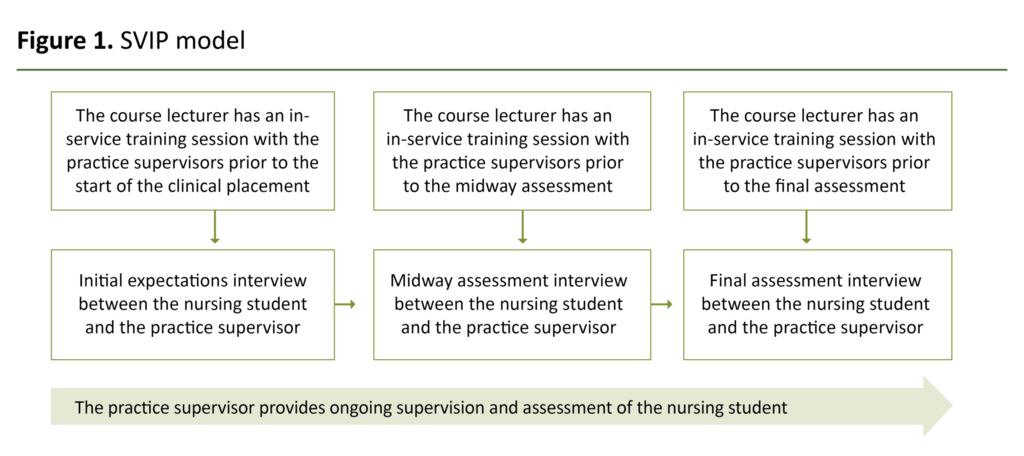
In the SVIP model, the practice supervisors meet the lecturer for in-service training three times during the clinical placement. These meetings take place at the placement institution prior to the initial, midway and final assessment interviews. In the in-service training sessions, practice supervisors share their experiences with supervising nursing students and receive guidance on their supervision.
The focus is on ensuring that nursing students have the opportunity to achieve the learning outcomes in their learning process. The lecturer provides guidance while the practice supervisor is responsible for clarifying the roles in the initial expectations interview.
At the midway and final assessments, nursing students evaluate their own efforts and are assessed by the practice supervisor based on an assessment form stating the learning outcomes for the subject. The practice supervisor and the student agree on the schedule for the assessment interviews. Students are responsible for preparing themselves for these assessment interviews.
The lecturer does not normally participate in the assessment interviews but is available if situations arise where the student or supervisor wants them to be there. Lecturers meet the students before the start of the clinical placement as well as at reflection groups during the period of practice.
In our study, the SVIP model was implemented over two periods of practice at four different psychiatric units in the specialist and primary health services. As far as we know, the SVIP model has not been tested previously in mental health nursing. Figure 1 illustrates the various meetings between the lecturer and the practice supervisor, and the practice supervisor and the student.
The objective of the study
The objective of the study was to examine how nursing students and practice supervisors perceive the SVIP model in clinical practice in mental health nursing.
Method
Design
We used a hermeneutic descriptive design and focus groups. Using focus groups is a suitable method for elucidating the shared attitudes and experiences of people in a given context or situation (20). In contrast to individual interviews, focus groups provide information through a dynamic group interaction process (21).
The hermeneutic approach allows the interview process to develop from the individual interview to an overall understanding, where the interview guide incorporates new questions in order to ensure in-depth knowledge about the experiences of the participants (21). In the analysis, we also compared the individual elements to the whole (22).
Sample and data collection
We conducted focus group interviews with nursing students and practice supervisors in clinical practice in mental health nursing in spring and autumn 2020, in the fourth and fifth semester. All nursing students and practice supervisors at the relevant placement providers were asked to participate and were given oral and written information about the project. Everyone who applied, took part in the project.
According to Polit and Beck (22), this constitutes purposive sampling, which means that the informants had experience of the SVIP model, thus ensuring in-depth knowledge of the objective of the study. The interviews were held at the university. We conducted seven focus group interviews – three groups of nursing students and four groups of practice supervisors.
The nursing students were women between the ages of 20 and 35, while the practice supervisors included one man and nine women aged 30 to 50. None of them had formal supervision qualifications but they all had previous experience as practice supervisors. There were two to four informants in each focus group. A focus group is characterised by interaction between the participants, which enriches the content (23).
Focus groups with few participants may result in a limited variation of experiences. Nevertheless, the validity of a focus group interview does not depend on the number of participants in the groups or the number of groups but on the richness and variation of the data collected (23).
The interviewers were experienced qualitative researchers. The third and fourth authors conducted the focus group interviews, with one of them leading the interview. The university lecturer following up the project in clinical practice did not take part in the interviews to ensure that the informants were not influenced by their presence. Audio recordings were made of the focus group interviews, and any identifiable statements in the recordings were anonymised in the transcriptions.
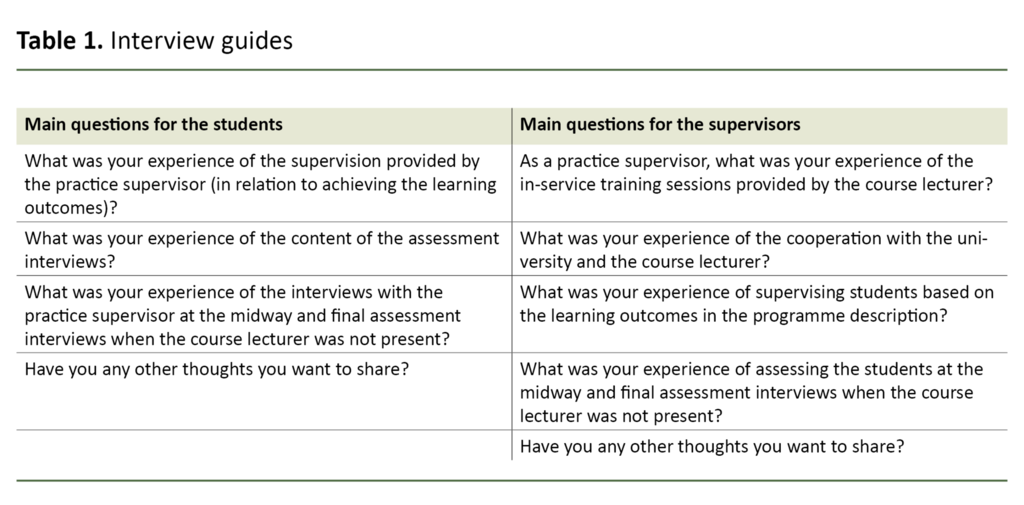
We used a semi-structured interview guide with open-ended questions. The authors devised the questions based on the objective of the study (21). The questions were adjusted in line with experiences gained in the first round of interviews. Table 1 shows the interview guides. The interviews lasted between 50 and 60 minutes.
Data analysis
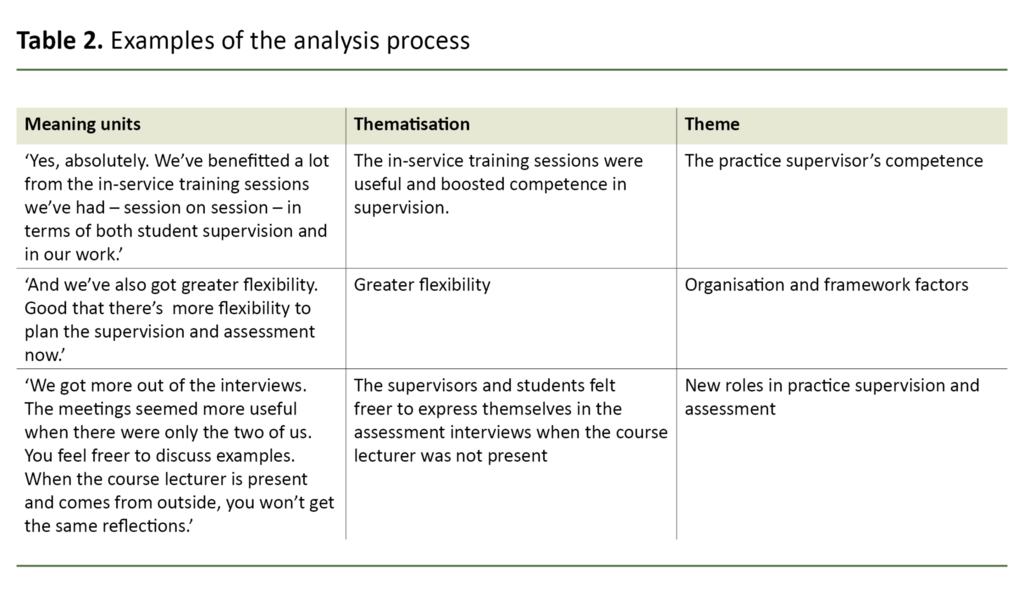
The transcribed interviews were analysed in line with Kvale’s content analysis (21). First, all the authors read the interview text in order to gain an overview. Then we identified the meaning units in the text using colour codes based on the objective of the study, and entered them in a table (Table 2).
These units were coded thematically, and we identified three main themes: 1) New roles in practice supervision and assessment, 2) The practice supervisor’s competence, and 3) Organisation and framework factors. The authors carried out this work jointly. We describe the findings in the results section, illustrating them with appropriate quotations and assigning them to the identified themes (21).
Ethical considerations
The informants gave written consent after being given oral and written information about the study. They were informed that participation was voluntary and that they could withdraw at any time. The informants were anonymised using letters and numbers, and a number was assigned to each interview. The nursing students were described as S2, S3, S6 and the practice supervisors as PS1, PS4, PS5, PS7.
We received approval from the university, the participating local authorities and the health trust to collect data. The project was approved by the Norwegian Centre for Research Data (NSD), reference number 591947. We used the SRQR checklist for qualitative research to ensure that each step of the research process was carried out correctly and in line with quality requirements.
Results
New roles in practice supervision and assessment
The lecturer’s role changed from that of having responsibility for assessment meetings with nursing students and practice supervisors to having a clearer role in providing guidance for the practice supervisors. Both nursing students and practice supervisors pointed to the need for roles to be clarified. The nursing students found it natural that the practice supervisor should be responsible for the assessment since the supervisor knew the student through shared experiences in their daily clinical work.
The presence of the lecturer was deemed to be disruptive since they were not familiar with the learning processes and situations that the practice supervisor and student had experienced together. Both students and supervisors were of this opinion.
One of the practice supervisors commented as follows: ‘We got more out of the conversations. The meetings seemed more useful when there were only the two of us. You feel freer to discuss examples. When the lecturer is present and comes from outside, you won’t get the same reflections’ (PS5).
One of the nursing students remarked: ‘The lecturer starts to talk and ask questions based on a written assignment you’ve delivered – it has a negative impact on learning. So as far as that’s concerned, SVIP has been a big improvement’ (S6).
When the practice supervisors had greater responsibility for the assessment, they became more familiar with the learning outcomes. Following the in-service training sessions with the lecturer, the practice supervisors were focussed on creating good learning environments, learning progression, structure and varied learning situations. Furthermore, they were motivated by their new responsibility and witnessed a positive development in the nursing students.
Both students and supervisors were worried about the potential development of a poor relationship between them. Nevertheless, they emphasised that knowing that the lecturer was available and that he/she would come to the placement setting if necessary, gave them a sense of security.
The practice supervisor’s competence
In their meetings with the lecturer, the practice supervisors systematically covered the learning outcomes in the programme description. Having the opportunity to reflect on them together with the lecturer was useful. They found that operationalising the learning outcomes and discussing the level expected of nursing students were necessary.
Moreover, the practice supervisors stated that there was a greater need for support from the lecturer. They felt that being given more responsibility for assessments also meant they had greater responsibility for the students’ learning process. The practice supervisors felt that the supervision skills they gained through in-service training were useful for the nursing students as well as for patient treatment and collaboration with colleagues.
As one practice supervisor said: ‘Yes, absolutely. We’ve benefitted a lot from the in-service training we’ve had – session on session – in terms of both student supervision and in our work’ (V1).
They also expected that the university would provide formal education in supervision that would enhance their competence.
The nursing students were generally satisfied with the competence of practice supervisors, finding that the supervisors benefitted from cooperation with the lecturer in the in-service training. The students had gained more knowledge of the learning outcomes and were better prepared when the SVIP model was used.
The nursing students found that the practice supervisors were more involved compared with previous clinical placements. They believed it was important that university staff valued the competence of practice supervisors, both supervision skills and clinical competence.
Organisation and framework factors
Both the practice supervisors and the nursing students believed that changes in the supervision model should be embedded in management at the placement provider so that time was scheduled and freed up for the practice supervisors to participate in in-service training. Some of the supervisors said that allocating time for supervision and assessment was not prioritised in shift planning despite the departmental management’s recognition and adoption of the new supervision model.
The nursing students stressed that practice supervisors should continue to participate in in-service training sessions with the lecturer, so that they became familiar with the programme description and the learning outcomes.
One nursing student said: ‘[…] so that the university and the placement provider have the same understanding. They don’t actually know what learning at my programme level is’ (S2).
A closer, more binding cooperation between the university and the placement provider, and between the lecturer and the practice supervisor was highlighted as an advantage. The SVIP model lay the foundation for better collaboration.
One practice supervisor commented: ‘I think the cooperation is much better than it used to be. Earlier, I think that communication was via the student and not directly between the lecturer and the practice supervisor’ (V7).
Both nursing students and practice supervisors emphasised that the SVIP model gave greater flexibility to plan and implement supervision and assessment. It was easier to change appointments when they did not need to involve the lecturer.
One of the students said: ‘We became freer to plan and change appointments according to what was best for the department’ (S2).
Another student also emphasised this: ‘I don’t understand. The lecturer just drops in at 11 am, right when you have a patient to take care of’ (S3).
Discussion
The objective of the study was to explore the experiences of nursing students and practice supervisors with the SVIP model in clinical practice in mental health nursing.
Clarification of roles in the new supervision model
The nursing students and practice supervisors had shared experiences of everyday situations in clinical practice. According to the students, it was logical that the supervisors were also responsible for the assessment. Both the supervisors and students wanted to have these conversations without the lecturer being present. This meant a change in responsibility for the practice supervisor.
Taking greater responsibility for the nursing students could result in more challenging tasks for the RNs in a health service already under pressure. The practice supervisors naturally prioritised patients over the supervision of nursing students (3), and this added to the stress (17). This challenge was also identified in the clinical practice project (4).
The different expectations attached to the RNs’ roles may lead to competing demands in respect of attention and responsibility (11). Roles must be clarified as a prerequisite for using the SVIP model in order to prevent role conflict. Both students and supervisors highlighted the need for this.
The clarification of roles and reciprocal expectations at an early stage was regarded as vital for a safe and stimulating learning environment. The findings in our study emphasise that the SVIP model can promote such clarification early in the placement period when the practice supervisor is given greater responsibility for both supervision and assessment.
The nursing students stressed the importance of the practice supervisor when it came to achieving the learning outcomes. Bogsti et al. (7) assert that it is the practice supervisor who seems to have most influence on the nursing students’ learning situation. When using the SVIP model, both students and supervisors experienced a closer cooperation. This led to the nursing students having a safe learning environment that stimulated their learning. They found that the practice supervisors had a greater and more focused sense of responsibility towards them when they also carried out the assessment.
This is in keeping with other studies showing that the relationship between the practice supervisor and the student is the key foundation of learning in practice (7, 24). Learning takes place in the interplay between a person’s social, cultural and material environment, as described in a socio-cultural view of learning in which social participation, dialogue and interaction are central elements (25). Moreover, learning focus depends on the recognition and acquisition of knowledge together with others.
Need for greater competence in supervision
The analysis of the interviews showed that the SVIP model could strengthen the competence of practice supervisors. In this model, the practice supervisor makes a formative and summative assessment of the student through daily supervision and a midway and final assessment (26). As experts in clinical practice, practice supervisors are well equipped to assess nursing students during placement periods (9).
Our findings show that practice supervisors need to be more familiar with the programme description generally, and supervision and assessment in particular. In a similar study, the participants also express a need for greater knowledge of the study programme (8).
Moreover, our findings show that practice supervisors gained more knowledge of the curriculum and the students’ learning process through the in-service training. Nordhagen et al. (8) found that in-service training with the practice supervisors promoted awareness of good learning situations and the criteria for skilled supervision.
When the role of the practice supervisors changed and they received a clearer responsibility for the nursing students, they needed more knowledge of supervision. One of the proposals put forward in the clinical practice project (4) was that a national model should be developed for a study programme in supervision. Such a model is considered an important measure for promoting the quality of clinical practice.
In 2018, regulations from Universities Norway (10) recommended a systematic enhancement of practice supervisors’ competence. Our findings reveal that putting focus on supervision reveals a need for more competence. If the SVIP model is combined with the opportunity to study for a formal qualification in supervision at an educational institution offering nursing education, the placement provider and the educational institution will form closer bonds.
Recognition of supervision competence is central to the SVIP model (8). Our study confirmed how important it is for the university to recognise the supervisor’s clinical competence as well. This will help to promote a good learning environment in a clinical context, a finding which is also reflected in other studies (27).
If educational institutions are to successfully introduce new supervision models that entail changes in roles, it is vital that this is embedded in management at the placement provider and the university. In-service training sessions between lecturers and practice supervisors promoted closer cooperation between the universities and the clinical placements, and can strengthen cooperation in terms of subject development and research going forward (28, 29).
Practice supervisors will naturally identify clinical questions that deserve further study. Together with university lecturers in the role of researcher, RNs can participate in different projects in the clinical setting. This can also help boost nursing students’ understanding of research (4).
Discussion of methodology
Malterud (23) is of the opinion that the ideal number of participants in a focus group is between five and eight. There were few participants in some of the focus groups in the study. Nevertheless, we believe that a rich body of material based on a dialogue between fewer participants in the focus group interview is valuable, even though the number of participants is not ideal. The participants contributed to enthusiastic discussions.
We devised four questions for the nursing students and five for the practice supervisors. We included a few open-ended questions in order to promote the informants’ own narratives so that we could follow up interesting lines of discussion in the conversation (23). The implementation of the project was limited to two periods of clinical practice at three placement providers. Nevertheless, we believe the findings can be transferred to other clinical practice situations.
Conclusion
The SVIP model challenges the traditional practice model. Reciprocal and binding cooperation between the university and the clinical placement is essential. The study shows that role clarification is vital and that the model must be embedded in management both at the placement provider and at the university. The practice supervisors’ clinical competence and need for enhanced supervision competence must be acknowledged in both arenas.
The focus by the Ministry of Education and Research and Universities Norway on boosting the quality of clinical practice nationally has shown that the SVIP model may be a step in the right direction. Several educational institutions are testing the supervision model, and it will be important to acquire knowledge and experience to boost the quality of clinical placements.
More qualitative and quantitative research is needed on the SVIP model. Research on the lecturer’s role is also needed.
The authors declare no conflicts of interest.






Comments