Guided Self-Determination as a tool in nursing consultations in primary healthcare – a literature study
Guided Self-Determination (GSD) can help improve the counselling skills of registered nurses. It can also encourage patients to reflect on their own communication skills.
Background: Lifestyle modification, in the form of a healthy diet, increased physical activity and appropriate medications, is necessary for people with type 2 diabetes mellitus (T2DM) to achieve good health, and thereby avoid late complications. Registered nurses (RNs) can support patients in remaining motivated in between their annual check-ups with their general practitioner. A good pedagogical tool can help ensure that conversations between RNs and patients are useful and that they help patients to master their condition.
Objective: To investigate the experiences of RNs and of people with T2DM of the RNs using Guided Self-Determination (GSD) as a pedagogical tool in consultations, and in the interval between conversations between patient and RN.
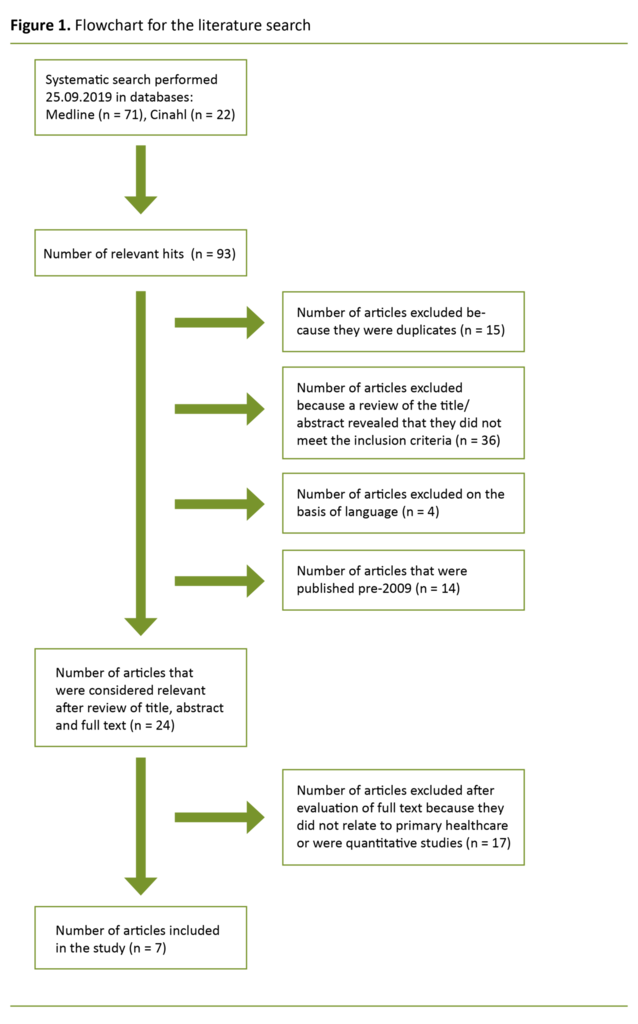
Method: We performed a literature search in September 2019 in the Medline and Cinahl databases for terms including diabetes mellitus type 2, self-management, empowerment, life skills, Guided Self-Determination, Self-Determination Theory, primary healthcare, nurse patient relationship and counselling.
Results: The search yielded a total of 93 hits, of which seven articles were included in the final literature summary. These show that the use of GSD can help improve the counselling skills of RNs, while also encouraging people with T2DM to reflect on their own communication skills. The approach can be challenging to learn, and RNs need time and experience to understand how best to apply the method. RNs felt that practicing the GSD method improved their skills as counsellors, while patients felt that they became more independent in managing their diabetes, and more aware of and engaged with their situation.
Conclusion: Both RNs and patients can benefit from the use of GSD in their conversations. However, the method should be further adapted to make it easier for RNs to use, and to enable more patients to benefit from it.
Type 2 diabetes mellitus (T2DM) results from a combination of insulin resistance – which is either hereditary or a product of lifestyle factors such as obesity and inactivity – and reduced insulin production in beta cells (1).
The number of people with T2DM is increasing worldwide as a result of ever-improving standards of living, easy access to food, reduced manual labour, and lower levels of physical activity. In Norway, between 260 000 and 280 000 people were estimated to be living with diabetes in 2020, of whom 90% had T2DM (2).
The national guidelines from the Norwegian Directorate of Health recommend that people with uncomplicated DMT2 should receive individual follow-up in the primary healthcare service as required, with a check-up by a general practitioner at least once a year (3).
Lifestyle modification, which emphasises a healthy diet tailored to the individual plus physical activity, is the cornerstone of T2DM treatment. However, for many patients lifestyle modification alone will not be sufficient to achieve treatment goals, and drug treatment will also be required.
Several major studies in general practice have shown that many patients do not achieve the recommended treatment goals (4), indicating a need for increased focus on what can be done to achieve these goals. Support from healthcare personnel has been shown to help individuals with T2DM make better day-to-day decisions about food, meals, and physical activity, and to more successfully adjust their medication on the basis of their blood sugar levels and thereby better manage their disease (5).
When following up individuals with T2DM, the use of an empowerment-based guidance tool can contribute to more effective and meaningful collaboration between nurse and patient.
Guided Self-Determination
There are a number of pedagogical tools available in healthcare. This article will take a closer look at Guided Self-Determination (GSD), which may be an appropriate method to use in patient consultations where problem solving and collaboration between patient and healthcare personnel has become difficult or where progress in treatment has stalled (6).
The GSD methodology was developed by Zoffmann at Rigshospitalet in Copenhagen (6) and has its origins in the Self-Determination Theory developed in Rochester in the USA (7). The method was developed as a way of improving decision-making and problem solving, and is intended for difficult diabetes care. The theory behind the method is based on empirical data (6, 8).
Through observation of conversations between patients and healthcare personnel, Zoffmann came up with three theories as to why healthcare personnel sometimes experience difficulties in using empowerment-based approaches with their patients (see fact box). Although healthcare personnel feel positively about empowering their patients, in practice it can often be difficult to mobilise strength and resources in an individual (9).
Zoffmann’s three theories are that healthcare personnel and patients may have differing perspectives on life and health; there may be conflict in the relationship between the two parties, and there may be differences in patterns of communication and reflection between patients and healthcare personnel (10).
Increases skills in diabetes management
GSD was initially developed as a tool for use in conversations between diabetes nurses and patients with type 1 diabetes mellitus (T1DM) (6). The method gave good results in terms of enabling patients to manage their diabetes more effectively, thereby reducing diabetes-related complications and improving glycaemic control (11).
GSD was then modified for use with other patient groups struggling with challenges associated with chronic conditions, such as adolescents with poorly controlled T1DM and their parents, young adults with poorly controlled T1DM, and patients with ADHD (12), schizophrenia (13), and chronic pain (14).
In several of these conditions, the use of GSD was shown to increase individuals’ self-management skills, with the result that they coped better with their illness. GSD is a pedagogical tool for healthcare personnel that is based on theories of perspective-taking, relationships, communication and reflection (10).
This improved ability to manage the disease and its treatment, along with better glycaemic control and fewer diabetes-related complications, resulted in positive outcomes with respect to achieving treatment goals (11).
This literature study aimed to investigate the experiences of registered nurses (RNs) and of people with T2DM, when the RNs use GSD as a pedagogical tool in their consultations.
Method
The methodology on which this article is based is the literature study (15); this involves selecting a topic, identifying a research question to address, and then performing a systematic literature search. The aim of the literature study was to describe the use of GSD as a pedagogical tool in nursing consultations in primary healthcare, by summarising studies that have planned or reported relevant experiences and perceptions (8).
Search strategy
PICO is a tool that is used to identify the key components of a clinical question (15). After selecting a topic, we used PICO to structure our research question and to identify suitable search terms.
The subjects in this study were patients with T2DM, and the intervention being evaluated was the use of GSD as a pedagogical tool in healthcare. Our aim was to look more closely at the experiences of RNs and of individuals with T2DM when the RNs use Guided Self-Determination (GSD) as a pedagogical tool in their consultations with patients and in the intervening periods.
To be included in this literature study, research articles had to include patients with T2DM who were followed up by the primary healthcare service, and focus on experiences related to the use of GSD as a pedagogical tool to promote the engagement of patients with their treatment. Relevant search terms in English were identified using the Medical Subject Headings (MeSH) database (15).
Searches were performed for each of the terms self-management, empowerment and life skills, as these are key terms in research on the GSD method. In addition, we searched for Guided Self-Determination and Self-Determination Theory. To expand or limit the search, we combined the search terms with AND or OR. We also combined the terms with primary healthcare, nurse patient relationship and counselling as part of our search strategy.
Literature search
We performed the literature search in September 2019 in Medline and Cinahl, which are important electronic databases for research in the field of nursing. These databases contain English-language articles on nursing, and are recommended for use within health and social care.
Both databases are recommended by Polit and Beck, and were chosen because they contain research on patient experiences and on the planning of studies in clinical practice that will improve understanding of experiences and perceptions related to the use of GSD in primary healthcare (15).
A total of 71 articles were identified by searching Medline, and 22 by searching Cinahl (Appendix 2 [in Norwegian]). After reviewing the titles and abstracts, we removed 36 of the 93 articles because they did not relate to the chosen topic and issue, and thus did not meet the inclusion criteria (Figure 1).
Studies performed in patient populations other than T2DM were excluded, as were studies featuring healthcare personnel other than RNs. We also excluded duplicates, as well as studies from non-Western cultures and in non-Western languages.
All authors read all seven articles, and systematically extracted information using a pre-specified list of information to be presented in the results section of the article.
GSD was developed over the period from 1996–2004 and has been in use in clinical practice ever since, while also being the subject of ongoing research and development. As the method has been constantly evolving, we excluded from this literature study any articles published more than ten years ago.
Fifteen articles did not relate to primary healthcare; another two articles did concern primary healthcare, but used a randomised controlled study design to measure efficacy. As a result, seven articles were included in the final analysis.
To assess the methodological quality of the articles, we used checklists published by the Norwegian Electronic Health Library (17) and assessment tools developed by the Critical Appraisal Skills Programme (CASP) (18).
Results
The seven selected articles (19–25) all have clear objectives and present their studies and findings in a clear and comprehensible manner (Appendix 1 [in Norwegian]). The aim was to investigate the experiences of nurses and of people with DMT2 with regard to the use of GSD as a pedagogical tool in healthcare.
This research has its origins in the increasing incidence of T2DM, and the interest in identifying what lies at the heart of good patient follow-up. The research studies were all conducted in the period between 2016 and 2019, with the aim of contributing to further development of GSD as a method for use in people with T2DM.
The study participants were RNs from the primary healthcare service who were employed at medical centres in southwestern Norway, and patients registered with those centres.
The research studies were approved by the Regional Committees for Medical and Health Research Ethics (REC) (20, 21, 23–25) or by the Norwegian Centre for Research Data (19, 22). The patients and RNs were all provided with information about the study, and those who participated gave written consent and were guaranteed confidentiality and the right to withdraw from the study at any time.
For the two studies that were approved by the Norwegian Centre for Research Data (19, 22), the parties involved had also received prior information, and their anonymity was ensured by removing names from the interview recordings and transcripts.
In five of the studies, RNs and patients were interviewed individually in face-to-face meetings with the researchers (19, 22–25), and in one study telephone interviews were used to contact the participants (21).
In all of the studies, two or more researchers transcribed and read the interview material. Then they identified the core messages and condensed the material, assigned codes to the various themes that emerged, and further divided the themes into subthemes. To ensure that the analysis was reliable, the codes, patterns and themes were discussed by the research team on multiple occasions.
Use of GSD in primary healthcare
In their article, Karlsen et al. (20) outline the protocol for future research. They wish to assess the effectiveness of a theory-based online GSD intervention in primary healthcare for adults with T2DM. They use various approaches to examine whether GSD can be beneficial for diabetes self-management and long-term glycaemic control (HbA1c).
Karlsen et al. report that moderate effects have been seen with previous interventions, and state that they wish to further develop the original GSD intervention. The study by Oftedal et al. (19) examines the experiences of nurses in learning to practise GSD and is among the completed studies described by Karlsen et al. in their study protocol (19). The remaining five articles (21–25) are all new work originating from the study protocol developed by Karlsen et al. (19).
The original GSD intervention, which was designed for people with T1DM and difficult diabetes care, consisted of seven face-to-face consultations involving 21 structured reflection sheets, and was intended to guide patients and healthcare personnel through mutual reflection.
Karlsen et al. (20) describe how they identified areas in the original GSD to be changed, and how they adapted the GSD programme to patients with T2DM. On the basis of findings from qualitative research, they reduced the number of consultations from 7 to 4, and the number of reflection sheets from 21 to 13, without losing any of the content (19, 23).
The modified GSD programme covers four themes: the patient–nurse relationship, life with diabetes, the relationship between ideal and reality, and work to achieve change (19, 20). This modified programme was then used as a starting point for an electronic version of GSD (20–22, 24, 25).
Using Minjournal.no, the communication service known today as Helsenorge.no, they conducted four consultations over a 12–16-week period and then interviewed the participants about their experiences of the online intervention (25).
What were the nurses’ experiences of using GSD?
The aim of the study by Oftedal et al. was to describe how RNs experience learning about and practicing GSD in primary healthcare among adults with T2DM (19). Four diabetes nurses from different medical centres received training in GSD in the form of a four-day course over nine months, with lectures, review of reflection sheets, workshops, discussions and supervisions. Once the RNs had completed the training and had been able to practice the method in their own workplaces, they were interviewed by the researchers. Analysis of these conversations revealed three main themes.
The first was that the RNs initially found the GSD method difficult to understand and to use. The nurses were to use communication skills known as mirroring, active listening and values clarification during consultations, but found doing so to be awkward and difficult. Eventually, as they gained more experience and received positive feedback from patients, they became more confident in their ability to understand the idea behind GSD and to apply the method in their own practice (19).
The second theme was that RNs required good training, with the use of concrete examples, to understand how to use the reflection sheets, and how to apply the communication techniques required.
The RNs emphasised that they had been missing a communication tool that they could use to help them succeed as counsellors.
Before being introduced to the GSD method, the RNs who were interviewed had planned their consultations with patients themselves. In their conversations with patients, they relied on what they had picked up as important from courses and guidelines. They emphasised that they had been missing a communication tool that they could use to help them succeed as counsellors. Although the RNs found the GSD method to be demanding, they recognised that GSD provided a structured approach and encouraged greater reflection (19).
The final theme that emerged was that the RNs felt they had developed during the process. Previously, they had been the ones who told patients what to do, but now it was the patients themselves who identified what would be beneficial for their health, and who came up with appropriate solutions in collaboration with the RN. The researchers refer to this as moving from a nurse-centred to a patient-centred approach (19).
Beginning with the modified electronic version of the GSD method developed by Karlsen et al. (20), Oftedal et al. (22) extended the work further by examining the experiences of nurses in using GSD in an electronic format. The online version involved fewer in-person consultations between patient and nurse and was based on asynchronous written communication (20, 22, 24).
On the basis of interviews with four RNs who had used the electronic version of GSD, the study concluded that the use of written communication may interfere with RNs’ ability to care for their patients. The authors note that non-verbal aspects of language, such as eye contact, facial expressions, posture and body language, are lost with written communication.
However, one of the RNs reported that face-to-face communication can be ‘noisy’ and can act as a barrier to reflective responses. The interviews also revealed that written communication can be a better means of tracking patients’ progress, as it enables both parties to read the reflection texts multiple times. One disadvantage, however, is that it is not possible to withdraw or make changes to the text, which can be problematic if a question has been misinterpreted.
It also emerged that written communication was time consuming, and that it was difficult to maintain professionalism through written feedback (22).
GSD from a patient perspective
In one study (23), which was part of the modelling phase of the study protocol developed by Karlsen et al. (20), researchers interviewed nine individuals with T2DM who had completed a face-to-face GSD intervention in general practice; the intervention had been modified from a more comprehensive T1DM programme.
The aim was to determine how these individuals had experienced the counselling process. The feedback from the participants was that they had become more aware of what it means to live with diabetes. Prior to the intervention, they had failed to come to terms with the fact that they had the disease, and this had also prevented them from making the necessary changes to their lifestyle.
Another theme that emerged was that through the GSD intervention, the patients found what they described as new resources in the disease. The counselling had enabled them to make their own decisions and to find ways of managing everyday problems.
The patients reported in the interview that they appreciated being seen and heard by the RN during the counselling process, and that the use of GSD increased the extent to which they viewed the RN as a conversation partner and a source of support and motivation. This in turn helped the participants to become more aware of the daily challenges of managing their disease, and as a result of the process they began to work on achieving goals that they had set for themselves during the GSD programme (23).
Through the GSD intervention, the patients found what they described as new resources in the disease.
Lie et al. (25) wished to examine patients’ experiences of using written reflection sheets as part of the online GSD intervention. Through ten one-to-one interviews, the authors identified two main themes. One was that written reflection can increase a patient’s awareness and engagement with their diabetes, both because writing creates the time and space for autonomous reflection, and because it encourages the individual to focus on self-management of their diabetes.
The researchers describe the GSD eHealth intervention as a double-edged sword, however, because their other main finding was that written reflection can sometimes be viewed as unhelpful in the self-management of diabetes. This is because, for many, writing is a difficult way to express oneself, and individuals may not always have the time or space to write down their reflections (25).
In a previous study, Lie et al. examined why patients chose to discontinue an eHealth intervention based on GSD (21). In all, 13 of 18 people who were invited to participate in the online GSD intervention dropped out, and this high drop-out rate formed the basis for the study.
It emerged that the patients who dropped out of the intervention lost motivation because they became frustrated with the technology, they found the content to be irrelevant and incomprehensible, or because they chose to pursue other activities and perspectives. The study also found that patients missed face-to-face consultations with an RN (21).
Both patients and RNs report that there are advantages to the use of eHealth interventions, but that they cannot fully replace conventional meetings between the two parties (22, 25). This formed the basis for a further study conducted by Lie et al. in 2019 (24).
In this study, the researchers looked at how the online GSD method affects the relationship between patient and RN, and found that it promotes greater mutual understanding and increased flexibility between the parties. But, as in their previous studies, they found that the use of written communication could affect the relationship between patient and RN as it allows for fewer face-to-face meetings, and because written communication can lead to misunderstandings and uncertainty.
In their study from 2018 (25), Lie et al. also found that physical meetings between patient and RN were important, because they enable, for example, patients to receive clarification on items in the reflection sheet that were difficult to understand.
Discussion
People with T2DM constitute a sizeable patient population. Self-management is crucial for these patients to master their illness and thereby accomplish their individual treatment goals and avoid late complications. Healthcare personnel must assess the skills, knowledge and not least the motivation of each individual. This is a crucial part of a counselling methodology such as GSD, which is tailored to individual patients and where the goal is to promote self-reflection and ultimately self-agency among patients with T2DM.
Karlsen et al. (20) refer to previous research showing that as few as one in eight patients with T2DM achieve the recommended treatment goals. A study conducted in general practice here in Norway in 2014 found that among a group of patients mainly with T2DM (of the 271 participants, 11% had T1DM and 88% had T2DM), only 13% achieved all recommended treatment goals, including HbA1c, blood pressure and LDL cholesterol (4).
As T2DM affects many people and is a disease in which it is difficult to achieve treatment goals, there is a need to develop pedagogical methods that can help improve consultations with this patient group. RNs must be provided with the skills and experience necessary to use tools in their consultations that are tailored to each individual patient and his/her specific needs. This is the essence of the GSD methodology.
The RNs improved their counselling skills
The articles in this literature summary emphasise the importance of working to improve nursing consultations, and the RNs who were interviewed in the studies stated that they had been missing a good pedagogical tool to use in their conversations with patients (19, 22). After receiving training in GSD, the RNs experienced an improvement in their skills as counsellors, and felt that the method encouraged individuals to reflect on their own communication skills (19).
This was also the conclusion of a Danish study that examined the effectiveness of training practice nurses in GSD. The nurses felt that the training allowed them to improve their skills in supporting patient autonomy. As many as 70% of the nurses who participated said that their skills in autonomy support improved, along with their communication skills (26–27).
Reflection sheets and communication techniques were difficult to use
The RNs interviewed in this literature study nevertheless felt that the GSD method was not easy to learn (19, 22). The reflection sheets consumed much of their attention during conversations with patients, and the RNs found them difficult to use (19).
Although the number of consultations and reflection sheets was reduced to better suit people with T2DM (20), it may be necessary to further modify the worksheets to make them easier to use during conversations.
Communication skills such as mirroring, active listening and values clarification were perceived as awkward and contrived.
The fact that communication skills such as mirroring, active listening and values clarification were perceived as awkward and contrived by the RNs (19), may indicate a need for changes in how RNs are trained in the use of GSD. The original training materials for GSD appear to address both theoretical and practical elements thoroughly (19), but it may nevertheless be necessary to consider how the communication skills can be made easier to learn and more natural for RNs to use in their consultations with patients.
For RNs to be able to use a new method in following up their patients, they must receive good training and the method itself should be manageable. It should be easy to understand and to apply without the point of the intervention being lost. The reflection sheets, which form an integral part of the pedagogical tool, should be shortened, for example, so that both RNs and patients find them easy to use.
GSD brings unspoken topics out into the open
In our training and at work, we are taught as RNs to show empathy and to listen to our patients, and to a lesser degree to challenge them in an appropriate way. The aim of GSD is to help us challenge our patients more. Patients reported that the GSD method and the reflection sheets increased their understanding of what it means to have diabetes and of how they could better live with the disease; they also reported feeling that they had been both seen and heard. This enabled them to become more independent in managing their diabetes (23).
Patients reported that the GSD method and the reflection sheets increased their understanding of what it means to have diabetes and of how they could better live with the disease.
The GSD method, which the article authors recognise has potential, also makes it easier to raise topics that would not previously have been discussed during conventional consultations (20). The meeting between patient and nurse changes from being based on measurements and results, to delving more deeply into the individual challenges faced by the patient, helping them gain greater awareness and, with support, to find their own ways of managing their situation.
These findings suggest that GSD touches on the goals of the underlying theories, namely of establishing a self-empowering relationship in the meeting between the patient and healthcare personnel (6).
Not everyone is keen on online technology
The traditional approach to treatment involving physical meetings with a diabetes nurse is today being challenged by new educational platforms. The use of online technology is highly relevant to areas including diabetes care. Articles on this topic show that eHealth interventions are useful tools in certain fields, but that they can also pose challenges (20–22, 24, 25).
A large number of patients dropped out of the eHealth version of the GSD intervention (21). Importantly, efforts were made to understand the reasons for this, so that the intervention could be adapted to reduce the number of people who drop out in the future. The fact that some found written communication difficult, or the technology frustrating (21), shows that the online version of GSD is not for everyone.
It is important to take this into account, and perhaps offer the online version as an alternative for those who feel that it is a good reflection tool, while using a version based more on spoken communication with those who are not keen on written or online communication.
The literature search was limited to articles describing experiences with the use of GSD, and there is much that remains unknown about the methodology. The small number of published articles, and the limited experience with the method in primary healthcare, are weaknesses of the study and limit the generalisability of the findings.
Further research is therefore needed in different study populations and settings, and not least larger and more extensive intervention studies to more systematically assess effectiveness. More information is needed about the use of GSD in medical centres and wellness centres, for example, and about which patients benefit most from the use of GSD in treatment. In addition, there is a need to consider how much can be invested in introducing this type of intervention into primary healthcare when the evidence base is so limited.
One must nevertheless conclude that eHealth interventions are here to stay, partly because of their continually improving and inspirational design, and partly because they represent a practical and easily accessible tool for communication and learning. Patients with somatic disorders can benefit from electronic interventions, and they can be both time- and cost-effective from a socioeconomic perspective (28).
Conclusion
Individuals with T2DM and diabetes nurses can both benefit from the use of GSD as an educational tool to stimulate reflection, decision-making and action, and as a means of empowering patients to master their illness. The experience of the RNs showed that the skills they gained as counsellors also encouraged them to reflect on their own communication skills.
Patients felt that they had been seen and heard, and they gained a better understanding of what it means to live with their disease. This in turn enabled them to achieve greater independence in managing their diabetes. Although writing down thoughts and feelings can stimulate reflection and bring forth new perspectives, it cannot fully replace face-to-face consultations.
References
1. Løvås K, Husebye E. Endokrinologi: en medisinsk lærebok. 2nd ed. Oslo: Gyldendal Akademisk; 2017.
2. Stene LC, Ruiz PLD, Åsvold BO, Bjarkø VV, Sørgjerd EP, Njølstad I, et al. Hvor mange har diabetes i Norge i 2020? Tidsskr Nor Legeforen. 12.11.2020. DOI: 10.4045/tidsskr.20.0849.
3. Helsedirektoratet. Nasjonal faglig retningslinje for diabetes, oppfølging, utredning og organisering av diabetesomsorgen og oppfølging av diabetes utenom årskontrollen. Oslo: Helsedirektoraret; 2018. Available at: https://www.helsedirektoratet.no/retningslinjer/diabetes/oppfolging-utredning-og-organisering-av-diabetesomsorgen/oppfolging-av-diabetes-utenom-arskontrollen (downloaded 21.01.2021).
4. Mouland G. Diabetes i en fastlegepraksis – ble behandlingsmålene nådd? Tidsskr Nor Legeforen. 2014;134:168–72.
5. Powers MA, Bardsley J, Cypress M, Duker P, Funnel MM, Fischl AH, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. The Diab Educ. 2017 feb.;43(1):40–53.
6. Zoffmann V, Hörnsten Å, Storbækken S, Graue M, Rasmussen B, Wahl A, et al. Translating person-centered care into practice: a comparative analysis of motivational interviewing, illness-integration support, and guided self-determination. Patient Educ Couns. 2016 mar.;99(3):400–7.
7. Ryan RM, Deci EL. Self-Determination Theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol Sci. 2000;55(1):66–78.
8. Malterud, K. Kvalitative forskningsmetoder for medisin og helsefag. 4th ed. Oslo: Universitetsforlaget; 2017.
9. Askheim OP. Empowerment i helse- og sosialfaglig arbeid – floskel, styringsverktøy eller frigjøringsstrategi? 1st ed. Oslo: Gyldendal Akademisk; 2018.
10. Zoffmann V, Kirkevold M. Realizing empowerment in difficult diabetes care: a guided self-determination intervention. Qual Health Res. 2012;22(1):103–18.
11. Zoffmann V, Lauritzen T. Guided self-determination improves life skills with type 1 diabetes and A1c in randomized controlled trial. Patient Educ Couns. 2006;64(1–3):78–86.
12. Enggaard H, Laugesen B, DeJonckheere M, Fetters MD, Dalgaard MK, Lauritsen MB, et al. Impact of the Guided Self-Determination intervention among adolescents with co-existing ADHD and medical disorder: a mixed methods study. Issues Ment Health Nurs. 2020 jul.;42(1):1–12.
13. Jørgensen R, Licht RW, Lysaker PH, Munk-Jørgensen P, Buck KD, Jensen SOW, et al. Effects on cognitive and clinical insight with the use of Guided Self-Determination. European Psychiatry. 2015 jul.;30(5):655–63.
14. Simonsen SM, Strømberg C, Zoffmann V, Hartwell D, Olesen ML. About me as a person not only the disease – piloting Guided Self‐Determination in an outpatient endometriosis setting. Scand J Caring Sci. 2019 des.;34(4):1017–27.
15. Polit D, Beck CT. Nursing research: generating and assessing evidence for nursing practice. 9th ed. Philadelphia: Wolters Kluwer Health; 2017.
16. MeSH på norsk. Begreper innen medisin og helsefag. Available at: http://mesh.uia.no/ (downloaded 27.06.2019).
17. Helsebiblioteket. Sjekklister for kritisk vurdering til bruk i systematiske oversikter eller forskningsprosjekter [Internet]. Oslo: Helsebiblioteket 03.06.2016 [cited 21.01.2021]. Available at: https//www.helsebiblioteket.no/kunnskapsbasert-praksis/kritisk-vurdering/sjekklister
18. The Critical Appraisals Skills Programme (CASP) CASP-Qualitative-Checklist-2018 [Internet]. Oxford: CASP UK 2018 [cited 21.01.2021]. Available at: https://casp-uk.net/casp-tools-checklists/
19. Oftedal B, Kolltveit BCH, Zoffmann V, Hörnsten Å, Graue M. Learning to practice the Guided Self-Determination approach in type 2 diabetes in primary care: a qualitative pilot study. Nursing Open. 2017;4(3):134–42.
20. Karlsen B, Oftedal B, Lie SS, Rokne B, Peyot M, Zoffmann V, et al. Assessment of a web-based Guided Self-Determination intervention for adults with type 2 diabetes in general practice: a study protocol. BMJ Open. 2016 nov.;6(12):1–9.
21. Lie SS, Karlsen B, Oord ER, Graue M, Oftedal B. Dropout from an eHealth intervention for adults with type 2 diabetes: a qualitative study. J Med Internet Res. 2017;19(5):e187.
22. Oftedal B, Kolltveit BCH, Graue M, Zoffmann V, Karlsen B, Thorne S, et al. Reconfiguring clinical communication in the electronic counselling context: the nuances of disruption. Nursing Open. 2018 okt.;1–8.
23. Karlsen B, Bruun BR, Oftedal B. New possibilities in life with type 2 diabetes: experiences from participating in a Guided Self-Determination Programme in general practice. Nursing Research and Practice. 2018 mar.;2018:6137628.
24. Lie SS, Karlsen B, Graue M, Oftedal B. The influence of an eHealth intervention for adults with type 2 diabetes on the patient-nurse relationship: a qualitative study. Scand J Caring Sci. 2019 sep.;33(3):741–9.
25. Lie SS, Karlsen B, Niemiec CP, Graue M, Oftedal B. Written reflection in an eHealth intervention for adults with type 2 diabetes mellitus: a qualitative study. Patient Prefer and Adherence. 2018 feb.;28(12):311–20.
26. Juul L, Maindal HT, Zoffmann V, Frydenberg M, Sandbaek A. A cluster randomized pragmatic trial applying self-determination theory to type 2 diabetes care in general practice. BMC Family Practice. 2011;12:130.
27. Juul L, Maindal HT, Zoffmann V, Frydenberg M, Sandbaek A. Effectiveness of a training course for general practice nurses in motivation support in type 2 diabetes care: a cluster-randomized trial. PLoS One. 2014 mai;9(5):e96683.
28. Elbert NJ, van Os-Medendorp H, van Renselaar W, Ekeland AG, Hakkaart-van Roijen L, Raat H, et al. Effectiveness and cost-effectiveness of ehealth interventions in somatic diseases: a systematic review of systematic reviews and meta-analysis. J Med Internet Res. 2014;16(4):e110.






Comments