Physical examination and health assessment by nursing students in clinical training
Background: Physical examination and health assessment (PEHA) has been an integral component in nursing curricula and professional development in recent years. PEHA training is intended to enhance nurses’ skills in the systematic collection of objective findings. It can also help them when evaluating and planning interventions.
Objective: In this study, we aimed to investigate the extent to which nursing students use PEHA skills in clinical training.
Method: In a cross-sectional study, nursing students at a Norwegian university were asked to complete an electronic questionnaire in their sixth semester. We present statistical analyses with a descriptive design. Free-text responses are categorised and presented thematically.
Results: A total of 75 nursing students answered the questionnaire. The respondents only practised 7 out of 20 PEHA skills regularly in relevant patient situations. Most PEHA skills (65%) are seldom or never used by nursing students in clinical training. The respondents highlighted the gap between theory and practice. They expressed that nursing supervisors lack knowledge of certain PEHA practices, which is a significant barrier to their clinical training.
Conclusion: Nursing curricula encompass a much broader range of clinical examinations than those regularly performed in clinical practice. The findings of this study can be used to inform the further development of nursing curricula. Consideration could be given to reducing the range of examination methods taught so that students can attain better proficiency in the methods used in clinical practice. If enhancing this competency in both present-day and future nurses seems beneficial, closer cooperation needs to be established between educational establishments and healthcare services. Studies are also needed into the correlation between the use of clinical examinations and students’ comprehension of and response to various clinical findings.
Cite the article
Lødemel I, André B, Brænd J. Physical examination and health assessment by nursing students in clinical training. Sykepleien Forskning. 2023; 18(94262):e-94262. DOI: 10.4220/Sykepleienf.2023.94262en
Introduction
The physical examination and health assessment (PEHA) method is based on four fundamental pillars of examination methodology: inspection, percussion, palpation and auscultation. It is argued that, through systematic observation of objective findings, this method facilitates early detection of conditions and prevents clinical deterioration (1).
PEHA skills can also provide nurses with a foundation for more precise reporting, as they gain a broader understanding of and can better describe the patient’s symptoms and medical problems. Nurses become familiar with multiple aspects of the clinical picture and gain a better understanding of doctors’ documentation (2). Developing nursing students’ clinical skills will improve patient care in the future (3).
PEHA in the bachelor’s programme in nursing
The core tasks of a nurse involve assessing patients’ individual needs for nursing care, implementing relevant interventions, and evaluating the efficacy of these together with the patient and other healthcare personnel. Using validated assessment tools undoubtedly improves patient safety as a result of early identification of changes in symptoms and clinical course. Such tools can also facilitate more precise documentation and communication among healthcare personnel (2).
Patient care and the nurse’s role are constantly evolving. A growing number of people will live significant portions of their lives with multi-morbidities. In order to address the demographic changes in society in general and within healthcare services specifically, new or expanded learning objectives are needed for nursing students. Nurses are increasingly encountering severe medical conditions that require nursing home or community nursing interventions. Improving nurses’ skills in the clinical assessment of frail patients in primary care settings is likely to reduce the number of unnecessary hospital admissions (4).
According to Norway’s regulations on national guidelines for nursing education, students should be able to apply knowledge of health and illness to systematically observe, assess, decide on, implement and document appropriate nursing interventions. They should also be able to evaluate the effect of these and make adjustments as needed (5).
These regulations highlight the importance of PEHA skills, but the wording of the clause leaves the expected level of knowledge and skills in bachelor’s programmes open to interpretation. Educational institutions are free to adopt different methods and practices in relation to this area of competency. The Norwegian University of Science and Technology (NTNU) introduced PEHA learning objectives in the bachelor’s programme in nursing in 2017 (6).
The goal of introducing PEHA was to enhance future nurses’ competence in comprehensive assessments and evaluations of the patient’s health status and needs, particularly within primary care settings.
Various terms are used to describe the methods nurses use to collect data during physical assessments of patients. In international research, terms used include ‘head-to-toe assessment’, ‘physical examination techniques’, ‘physical examination and health assessment’ and ‘physical assessment skills/techniques’ (2, 7).
In Norwegian nursing literature and research, as well as in the field of practice, there is no established consensus on what physical examination and health assessment entails. Different terms and acronyms are used for nurses’ clinical assessment of the patient. Monitoring vital parameters was an important component in nursing curricula long before the introduction of PEHA. The National Early Warning Score (NEWS) is one of the tools included in PEHA. This tool is validated for identifying exacerbations in a variety of conditions and facilitates concise communication between healthcare personnel (8).
NEWS is a recognised tool, particularly for assessing the course of infection and sepsis and sepsis-related organ failure (9). In Norway, NEWS was introduced as part of patient safety efforts through the initiative ‘Early detection of clinical deterioration’, and has now been included in national clinical guidelines from the Norwegian Directorate of Health (10). However, PEHA differs from NEWS in that PEHA encompasses more than the monitoring of vital parameters and has a focus on the physical examination of all organ systems (2, 4).
Purpose of the study
The PEHA method primarily systematises examinations that are well-known within nursing but also includes methods that have not traditionally been part of the nursing role. More advanced examination techniques involving percussion and auscultation have traditionally been the preserve of doctors, and still are to a large extent.
Clinical examinations such as auscultation and percussion of the lungs, heart and abdomen were incorporated into nursing curricula relatively recently. Nurses are not, however, expected to be able to make a diagnosis, but they should be able to distinguish between normal and abnormal findings.
The curriculum requires nurses to actively apply their acquired skills in practice. The long-term goal is for nurses to use PEHA in clinical practice, but changing the nursing role takes time. Insufficient hands-on experience with the method during clinical training may prevent the transfer of skills to their roles as qualified nurses. Consequently, the knowledge they have acquired is more likely to fade after the end of their studies. In order to investigate whether the curriculum is tailored to clinical practice, we posed the following research question:
‘To what extent do nursing students use PEHA skills in clinical training?’
Method
Design of the study
We conducted a cross-sectional study using the University of Oslo’s Nettskjema questionnaire. Third-year students in the bachelor’s nursing programme at NTNU were invited to complete an electronic questionnaire (Appendix 1 – only in Norwegian) (11). The survey focussed on students’ use of the various examination and assessment methods that had been covered in the PEHA component of the curriculum. The survey also included free-text questions about students’ experiences with applying this knowledge in clinical training, as well as the barriers to doing so.
The selection of examination and assessment tools taught in the bachelor’s programme in nursing at NTNU is based on a study by Nord University (2) that summarises previous research on which examinations nurses perform internationally, including in the United States and Australia. PEHA is defined as a comprehensive physical examination by means of inspection, palpation, percussion and auscultation, in addition to psychological and mental health screening (2, 12).
Our study encompassed 20 core PEHA skills in the bachelor’s programme in nursing curriculum at NTNU. The selection represents various techniques within inspection, palpation, percussion and auscultation, as well as head-to-toe assessment, pain assessment (NRS and MOBID-2), screening for anxiety and depression (GAD-7 and PHQ-9, respectively), systematic data collection of vital parameters (NEWS), mental status assessment (ABCT) and level of consciousness assessment (ACVPU and GCS).
We formulated the questions to capture the frequency of students’ reported use of the various skills in relevant patient situations during five clinical placements, each lasting eight to ten weeks. The following is a sample question from the questionnaire: ‘How frequently do you perform ‘auscultation of the lungs’ when assessing a patient’s lung condition?’
The response alternatives are based on a Likert scale (0 = Never, 1 = Very seldom, 2 = Seldom, 3 = Often, 4 = Very often, 5 = Routinely) (17). In the results, average and median scores of ≥ 2.5 indicate regular use and < 2.5 indicates infrequent use of the techniques.
The results were analysed in SPSS, version 28, and are presented with a descriptive design, including mean scores with corresponding standard deviations and median scores with corresponding interquartile range. Free-text responses were analysed categorically and presented thematically along with some representative quotes.
Sample
On 25 February 2022, the questionnaire was emailed to third-year students (n = 193) taking a bachelor’s degree in nursing. The deadline for submitting the completed questionnaire was 15 March 2022. Most respondents completed the questionnaire electronically during a class lesson. The sample of respondents was mostly made up of the students who attended this lesson.
The respondents were asked to base their answers on their experiences at all five of their clinical placements in nursing homes, community nursing, mental health care and surgical and medical wards. A total of 75 nursing students in their sixth semester (38.9%) completed the questionnaire and were included in the study.
Ethical reflections
The data collected are anonymised and do not therefore contain information that can identify individuals, either directly, indirectly or through an email or IP address or an identifying key. Use of the Nettskjema form ensured anonymity (11).
It was not possible to identify individuals at any point during data collection. There was therefore no requirement to notify the Norwegian Agency for Shared Services in Education and Research (Sikt) of the project or to seek any other type of approval. We informed the respondents about the purpose of the study, voluntary participation and anonymity in an information letter that was emailed to them along with the invitation to participate in the study.
Results
The results regarding students’ application of PEHA skills in relevant patient situations during clinical training are shown in Table 1. Seven out of the 20 PEHA examination techniques are regularly used by the respondents (median = 3–5, mean score = 2.53–4.80). Thirteen of the 20 are seldom or never used (median = 0–2, mean score = 0.47–1.87).
Examinations and assessments of vital parameters, pain assessments using the NRS, level of consciousness assessments using ACVPU, and inspections of the oral cavity were among those most frequently performed.
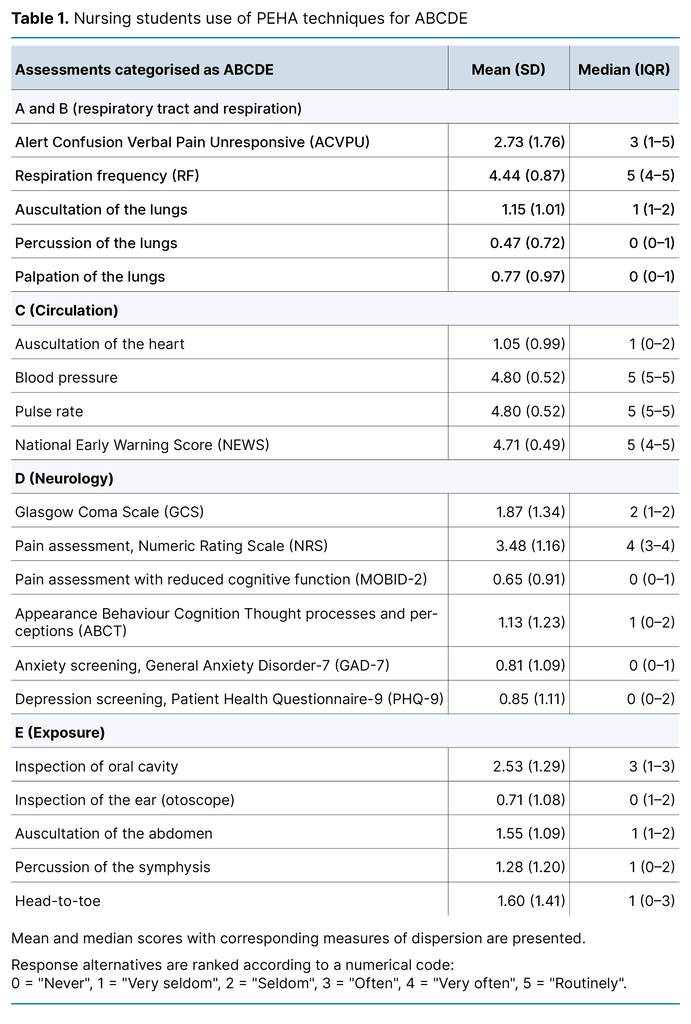
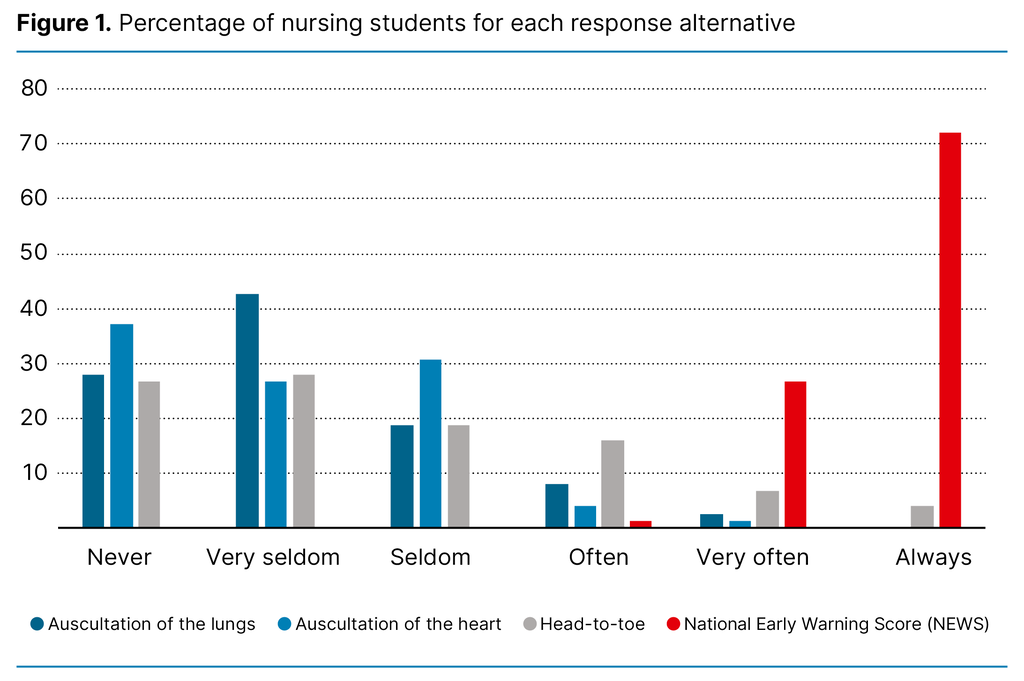
NEWS appears to be the most frequently used tool, with 71% of respondents indicating that they always use this for the systematic collection of data on vital parameters. All respondents stated that they use the tool often or routinely in relevant patient situations. In comparison, 88% of respondents seldom auscultate the lungs, 93% seldom or never auscultate the heart, and 72% seldom or never perform a head-to-toe examination (Figure 1).
Seventy-five of the respondents agreed or strongly agreed that they have a good understanding of what PEHA entails and in which patient situations the various examination techniques are useful.
In response to the statement suggesting that the theoretical knowledge they had learned on PEHA provided them with sufficient competence to perform and practise the examination methods in clinical training, 52% of the respondents disagreed or strongly disagreed, while 48% agreed or strongly agreed. Furthermore, 57% reported being comfortable explaining what PEHA entails to colleagues in the field of practice.
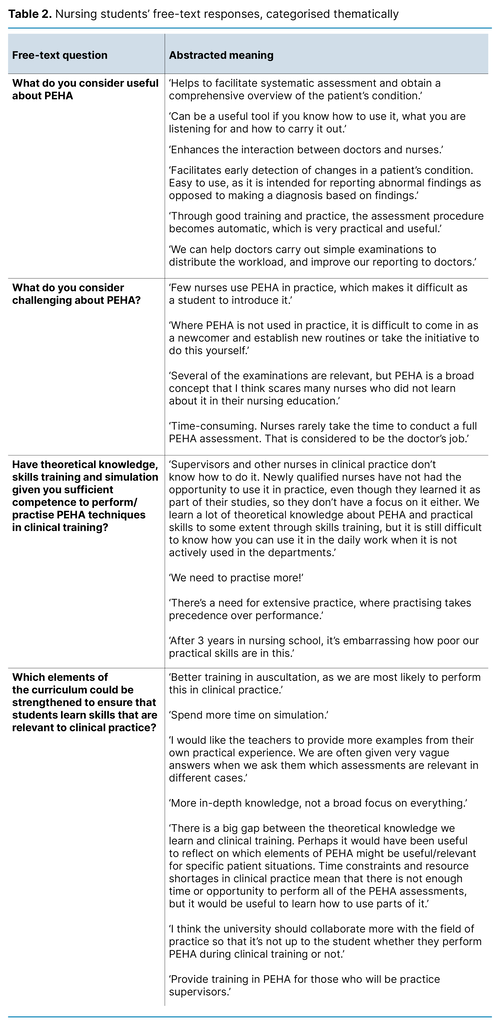
Several respondents argued that PEHA was useful for obtaining a comprehensive overview of the patient’s condition and facilitating interaction between nurses and doctors. They also expressed that there were several barriers to using PEHA techniques. Some believed that few nurses in clinical practice use PEHA and that they do not have the time to do so. Several of the examinations were considered part of the doctor’s remit, making it challenging for the students to introduce new routines in clinical practice (Table 2).
Discussion
The respondents reported regularly performing examinations and assessments of the patient’s level of consciousness, vital parameters, and using the NRS self-reporting tool to assess pain in clinical training. However, they seldom or never used the study’s other PEHA techniques in clinical training.
Nursing students’ use of PEHA
The respondents consider PEHA to be a useful tool for conducting comprehensive patient assessments, enhancing the interaction between doctors and nurses, and quickly identifying clinical deterioration.
Respondents reported using 35% of the study’s examination techniques in relevant patient situations in clinical training. The PEHA examinations most frequently performed are included in NEWS, such as measurements of respiratory rate, oxygen saturation, blood pressure, pulse rate, level of consciousness (ACVPU), temperature and subjective pain (NRS).
A significant proportion of the PEHA examinations in the study were not performed by the respondents in clinical training. This finding is not surprising when compared to research in countries with more experience in advanced clinical examinations in nursing care. An Australian study (13) shows that only 34% of the examination techniques that nurses learn are regularly used in practice.
A study from the United States (14) found that nurses used 30 of the 126 surveyed examination methods regularly. Core techniques in inspection and general observation were heavily overrepresented in the physical assessments, and one-third of the methods used were related to cardiovascular and respiratory assessments.
An Italian study of nurses in intensive care units and medical and surgical wards showed that 20 out of 30 core physical assessment techniques were used regularly. Auscultation of heart, lung and bowel sounds was seldom or never performed (15).
Other studies have similar findings (7) and question whether it is appropriate to teach nursing students a broad range of advanced clinical examination skills that are not used in practice. This argument is supported by a Norwegian study by Egilsdottir et al. (16), who studied a selection of 30 assessment techniques covered in the Norwegian nursing curriculum: Basic Physical Assessment Skills (B-PAS). They found that auscultation and percussion were among the skills that were seldom used in clinical training (16).
Factors of significance for the application of PEHA in the clinical setting
One of the barriers highlighted by the respondents is that only a small number of nursing supervisors perform PEHA in practice. This limited access to role models with proficiency in such methods limits students’ opportunities for guidance. Nursing students are taught not to diagnose patients, but they should be able to distinguish between normal and abnormal findings in order to further document a patient’s health status and report this to a doctor or other health personnel.
Nevertheless, the respondents found it challenging to initiate patient assessments that are not considered part of the nurse’s remit. Barriers to using PEHA as a working method are linked to time pressure, constant disruptions to their work, the absence of common practice, a lack of role models in the nursing profession with proficiency in the methods, lack of confidence in own clinical skills and unclear demarcation lines between nurses and doctors (17).
The respondents suggest training practice supervisors and establishing closer cooperation with the field of practice in order to enhance PEHA competence in clinical practice. Results from a Norwegian study by Bing-Jonsson et al. indicate that healthcare personnel in nursing homes and community nursing services have insufficient competence in comprehensive assessments and advanced procedures to provide the necessary health care (18).
Training nursing students in PEHA can be considered a means of reducing the gap between the expected and actual competence of nurses in primary care settings. However, the differing approaches to comprehensive clinical assessment in practice and in the nursing curriculum present challenges for nursing students (19).
The results from our study show that nursing students need extensive practice in the various skills. The respondents also call for clarification of the context in which some or all PEHA methods should be used. About half of the respondents felt that the PEHA component of the curriculum did not provide a sufficient foundation for practising these skills in clinical training. The nursing students expressed a desire for more training in auscultation as this is considered a potentially valuable skill in clinical practice. Studies have shown that skills in auscultation of the lungs, heart and abdomen are mainly developed through clinical practice and the associated reflection on the patient’s health status (20, 21).
However, it is unclear whether nurses’ use of PEHA impacts on patient outcomes and patient safety (22). Auscultation of the heart has been found to have limited accuracy in detecting heart disease in asymptomatic patients and is considered a poor diagnostic tool for doctors in primary care settings. Easy access to echocardiography is proposed as a more patient-safe strategy for patients exhibiting symptoms of coronary disease (23).
The respondents considered PEHA potentially useful for the field of practice. They argued that PEHA can contribute to a prompt and comprehensive assessment of the patient’s condition, early detection of clinical deterioration and improved workflow and interaction with the doctor. Previous research has shown that nurses with advanced clinical skills feel that they would not be able to identify serious developments in the patient’s health without this competence. Experience and practice also lead to a deeper understanding of the causes of and correlations between symptoms and illness progression (24).
Nurses involved in training nursing students in clinical practice, however, consider there to be shortcomings in their professional capabilities to provide guidance. They express that it is difficult to keep abreast of the students’ curriculum and learning objectives and to effectively apply the theoretical knowledge in practice (25).
Nurses with competence in using PEHA methods as a basis for assessment will be well-equipped for clinical practice in various parts of the health service. Academic learning that is relevant to practice prepares nurses for performing relevant examinations and interpreting the results. This enhances their clinical competence and confidence, thereby improving patient care (3).
Reflections on methodology
The questionnaire in this study has not been validated for use but is inspired by previous studies in the field (3, 13, 14, 26). We used a Likert scale for the response alternatives with a view to measuring self-reported use of PEHA methods.
The low response rate (38.9%) means that the reliability of the results must be interpreted with caution.
One of the weaknesses of using a questionnaire to collect data is that respondents can interpret the questions and response alternatives differently (17). However, the questions were formulated in a way that minimises misinterpretation. The study is limited to a selection of clinical examinations and does not encompass all the tools and methods taught as part of the nursing curriculum. This is because we wanted to gain an insight into the practical skills acquired by nursing students through their use of different PEHA methods.
The study concerns the examinations and assessments covered in PEHA in the relevant nursing curriculum. The findings of the study may be influenced by the institution’s approach to teaching PEHA and may not therefore be fully generalisable to institutions employing other approaches.
The findings primarily shed light on the gap between theory and practice and highlight the challenges of learning PEHA techniques in clinical training. This is particularly relevant where the practice supervisor does not have competence in this area. The study’s findings can raise awareness and stimulate reflection that can be valuable when developing nursing curricula. They can also help to inform the discourse on the potential task-shifting implications for nurses’ areas of responsibility as a result of their application of PEHA.
Conclusion
Effective strategies should be incorporated into nursing curricula for introducing students to clinical examinations. Their progression through the bachelor’s programme should be realistic and relevant. Closer cooperation with the field of practice is needed to strengthen the supervision of nursing students in clinical training. Nurses who have not been taught PEHA as part of the nursing curriculum must be given the necessary training. NTNU is currently offering external courses in PEHA for nurses in the health service.
The societal mission of nursing education is to develop knowledge and competence that is useful for the health service. However, introducing new elements in the curriculum, such as PEHA training, to clinical training without adequate preparation of practising nurses will widen the gap between academic learning and clinical practice.
The study shows that students are not achieving the intended learning outcomes for PEHA. If the teaching of PEHA is more tailored to the needs of different patient groups, students would have a better understanding of when to use components of PEHA in specific patient situations. Increasing the focus on integrating theory and practice can facilitate students’ learning and proficiency.
If the teaching of PEHA is adapted to a more realistic level and scope, it may enhance students’ comprehension and confidence in applying this method. This will increase the likelihood of the learned knowledge being incorporated into nursing practice and prevent it from fading after the end of their studies.
More knowledge is needed on how nurses’ use of PEHA impacts on patients’ health, and to what extent it facilitates good decisions about treatment. Nurses bear a particularly significant responsibility when low sensitivity methods are employed in cases where this has implications for the assessment and the decision on whether to consult a doctor.
If nurses perform clinical examinations that were previously the preserve of doctors, and no abnormal findings are detected in a sick patient, this could increase the risk of treatment delays or omissions. It also entails the nurse assuming more clinical responsibility. We believe there is a need for studies that further examine the correlation between the application of PEHA and students’ comprehension of and response to various clinical findings.
The authors declare no conflicts of interest.
Open access CC BY 4.0
The Study's Contribution of New Knowledge

Most read
Doctorates
Selvrealisering og betydning for helsesykepleieres fortsatte yrkesutøvelse. En kvalitativ studie.
Dårlig samvittighet hos sykepleiere - En multimetodestudie om sykepleieres erfaring med dårlig samvittighet i sykehjem og hjemmebasert omsorg
Helserelatert livskvalitet og mental helse etter ekstremt prematur fødsel
Å leke med dukker i sykepleierutdanningen





















Comments