Training in shared decision-making for registered nurses taking a master’s degree and/or a postgraduate programme
Registered nurses taking a master’s degree and/or a postgraduate programme acquired relevant knowledge that they could use in their daily work in order to assist patients in the decision-making process.
Background: Registered nurses play a decisive role in supporting patients to participate in decisions on their own health, also referred to as shared decision-making. Official recommendations and up-to-date knowledge demonstrate that, although shared decision-making is necessary for patients, there are few training programmes within or outside the education system that can meet this need for competence.
Objective: To gain insight into how RNs taking a master’s degree and/or a postgraduate programme respond to a three-hour training module in SDM and decision coaching, and how students perceive the effect on learning. We also wanted to identify possible barriers and facilitators in relation to the use of decision coaching.
Method: We used a multi-method research design based on Kirkpatrick’s four-step model for evaluating training interventions. We reported on the first two levels – reaction and learning – using a questionnaire to assess how students reacted to and learned from the training. The quantitative data were analysed using descriptive statistics, but we analysed the free-text questions using qualitative content analysis.
Results: Eighty-two registered nurses taking a master’s degree and/or a postgraduate programme in cancer nursing or nephrology nursing participated in the course, and 76 of them consented to take part in the study. The registered nurses reported that the teaching was useful for clinical practice and recommended it to others. They also wanted more skills training in order to increase their competence in shared decision-making. They highlighted the ‘Six steps to shared decision-making’ in addition to role play and exercises as among the most useful elements of the training. A broad spectrum of barriers and facilitators across individual, organisational and systemic levels were reported.
Conclusion: The study shows that the registered nurses found that the training provided them with relevant knowledge that they could use in their daily work in order to promote the development of knowledge about the shared decision-making process. Further training is both desirable and necessary in order to increase registered nurses’ self-confidence and skills in practising decision coaching.
Introduction
User involvement means that ‘those who are affected by a decision or are service users have influence on the decision-making processes and the design of the service provision’ (1). At the individual level, user involvement is effectuated through dialogue between the patient and healthcare personnel in which the patient has the opportunity to contribute, including participating in choosing between different kinds of screening or treatment methods (2).
In recent years, shared decision-making (SDM) has attracted increased attention. Both ethical guidelines and health policy guidelines clearly indicate that patients should participate in decisions about their own health (3–5). SDM is recommended as a method of enabling patients to become more involved in decisions about their own health (3, 5).
Special SDM tools can support the patient by giving complete, comprehensible information about the desired effect of the treatment alternatives, as well as the side-effects and complications, and their frequency (6).
A ‘decision coach’ is a healthcare professional who is trained to provide support to patients who face such a decision, so that they can make an informed choice (7). In spite of a number of measures that have been developed to make SDM more widespread, research shows that patients are still not sufficiently involved in decisions about their own health (8, 9).
Even though an increasing number of studies evaluating the effect of training interventions have been published, it is not clear what best practice is (10). The variation in evaluation methods and the teaching itself make it difficult to identify the ‘active ingredients’ (11–13) and define the necessary course length and learning method (12). Moreover, the literature shows that existing training programmes have not been evaluated to a sufficient extent and do not have clear enough didactics and concepts (12).
To meet the need for knowledge-based skills enhancement through courses with different formats and lengths in Norway, the module-based framework ‘Ready for SDM’ has been developed (3, 14–16).
The aim of ‘Ready for SDM’ is to promote the implementation of SDM. This is done by strengthening healthcare personnel’s competence in involving patients in decisions about their own health so that more patients make informed choices in conjunction with healthcare providers. This will boost the quality of the decision-making conversations.
The framework is based MAPPIN’SDM (Multifocal Approach to Sharing in SDM), a quality concept for service user involvement in decisions (9, 17). MAPPIN’SDM defines the steps in the SDM process chronologically, and provides detailed descriptions of several performance levels for each quality indicator (9, 17). The conceptual criteria follow ethical guidelines and legislation (2, 19), as well as guidelines on when and how patients should receive information and be involved in decisions (20).
‘Ready for SDM’ consists of several training modules in different formats allowing them to be tailored to the needs of the target group. The target groups include registered nurses (RNs), doctors, students and decision coaches.
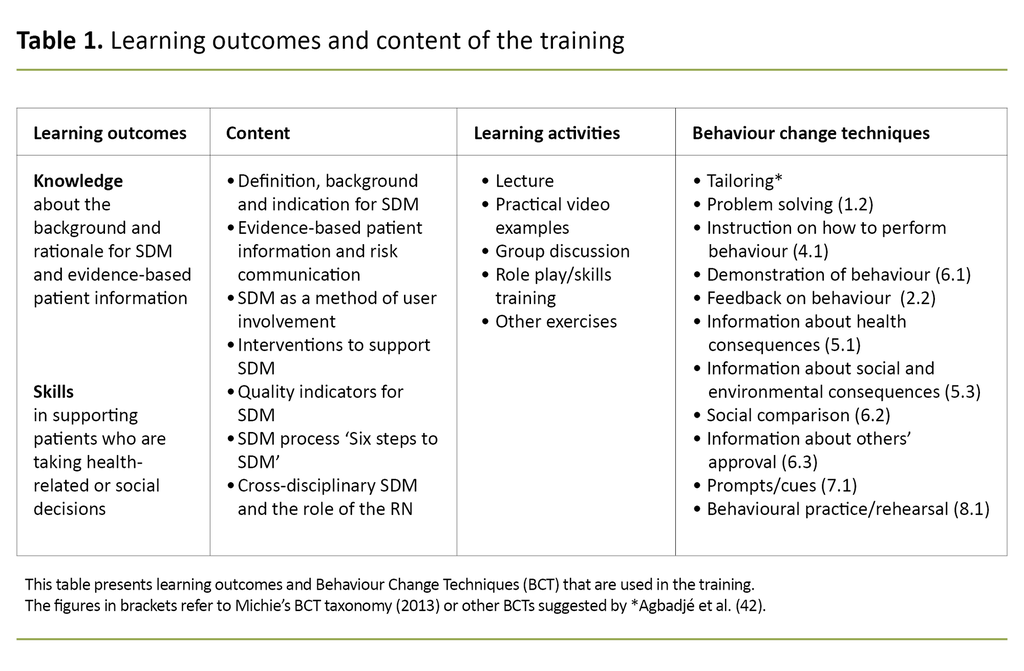
The Ready for SDM meta-curriculum (15) uses a generic pedagogical approach in addition to different behaviour change techniques (BCTs), an evidence-based taxonomy of 93 hierarchically grouped BCTs. The aim is to create international consensus for reporting behaviour change interventions (13). The BCTs are defined as components of an intervention that are observable and replicable, irreducible and designed to change behaviour (Table 1).
RNs play a decisive role in supporting patients to take part in decisions (7), but there seems to be considerable variation in the extent to which students taking a master’s degree and/or a postgraduate programme receive training on the topic (21–23). SDM is mentioned in connection with the new national guidelines for Norwegian health and welfare education (RETHOS 1), where SDM is to be given more prominence in undergraduate nursing education (18).
The aim of the guidelines is to ensure that study programmes are future-oriented and in line with the competence needs of the healthcare services and service users. These guidelines can help to prepare students for patient interaction and the challenges of clinical practice. Research shows that effective interventions are needed to make SDM more widespread. One such measure might be that RNs boost their competence to enable them to give better support to patients faced with decisions.
VID Specialized University and the Inland Norway University of Applied Sciences are two Norwegian universities that have expressed a wish for a training module for students in master’s and/or postgraduate programmes in cancer and nephrology nursing. RNs in cancer and nephrology care are faced with many issues where SDM is relevant.
In cancer care, the patient and their families can be confronted with very challenging and unfamiliar choices when a decision on a treatment pathway has to be made. The conversation about this often takes places shortly after the diagnosis is made, at a time when the patient and their family may be unprepared for both the diagnosis and the degree of severity. The patient’s encounter with the treatment programmes and a possible cancer diagnosis may be characterised by emotional crisis, confusion and anxiety that may prevent them from comprehending the information given as well as the options (24).
The patient may be faced with choices between the treatment alternatives that are available and justifiable throughout the patient pathway (2), and it may therefore be appropriate to have a decision-making conversation. This also applies to the treatment of patients with chronic kidney disease. The issues of concern range from the choice of dialysis, diet restrictions, discontinuation of dialysis and preparation for the end-of-life phase. For example, in the case of severe kidney disease, the choice is between haemodialysis or peritoneal dialysis, kidney transplant or conservative treatment.
While decisions in cancer care often need to be made suddenly and entail time pressure as well as the processing of bad news, the decision-making process for chronic disorders is slower. SDM is relevant in both the so-called one-off decisions and long-term decisions, whereby decisions are repeatedly made in the course of the patient pathway.
Objective of the study
The objective of this study was to gather knowledge about how RNs taking a master’s degree and/or a postgraduate programme respond to a three-hour training module in SDM and decision coaching, and how students perceive the effect on learning. We also wanted to identify possible barriers and facilitators in relation to the use of decision coaching.
Method
Design
We used a multi-method design based on Kirkpatrick’s model for evaluating training interventions. It structures the evaluation of the training intervention on four levels, and can be used for different studies and methods (25).
Level 1 deals with the evaluation of the participants’ immediate reactions, and encompasses both relevance and satisfaction. Level 2 deals with the participants’ learning during the training module and includes the development of knowledge and competence in addition to changes in attitudes. Level 3 evaluates the actual change in behaviour after the intervention. Normally, separate studies are conducted to evaluate level 4, where the focus is on patient-relevant outcomes. It may be useful to refer to the level evaluated by the study in order to facilitate comparison of studies.
Our study examined the participants’ perception of the relevance of the training module and their satisfaction with the training (level 1), as well as their knowledge, attitude to patient involvement, self-confidence and commitment in relation to carrying out SDM themselves (level 2).
Sample
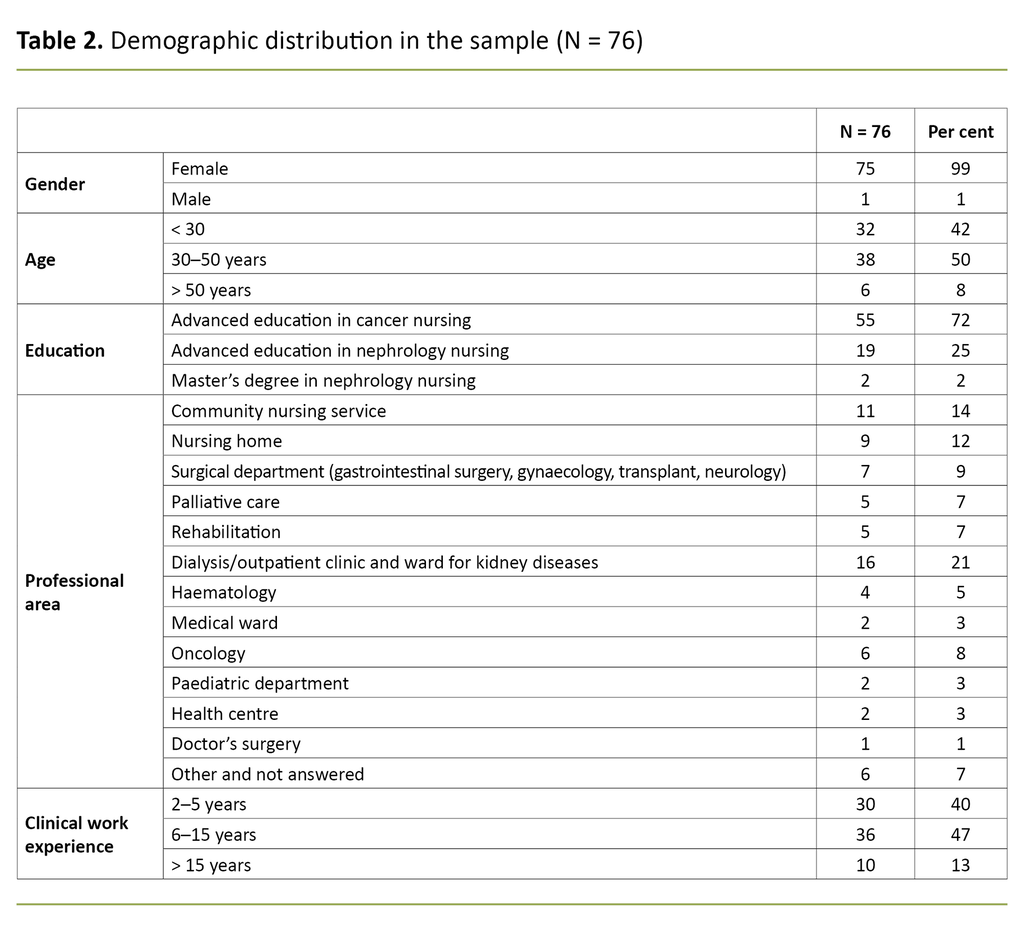
In autumn 2020, we invited all the 82 students participating in an SDM training module at VID Specialized University in Oslo and the Inland Norway University of Applied Sciences in Elverum to take part in the study. A total of 76 students (93 per cent) consented to participate, and all of them provided the necessary data. Sixty-four students (84 per cent) took part in the teaching in person while the remaining twelve participated remotely (16 per cent).
Training module
The training was based on the Ottawa Decision Support Frameworkand an international model for interprofessional SDM (26, 27), which formed a theoretical basis for positioning and explaining the RN’s role in an SDM process. The development team devised a training module by combining different teaching methods (28). Learning activities and BCTs from the meta-curriculum were used. (15, 16, 29).
The training module lasts three hours, and the basic model, i.e. the first two hours, is used to introduce students to SDM (15, 16) (Table 1). These two hours have already been evaluated as being acceptable, useful and relevant for the target group (15, 16, 29).
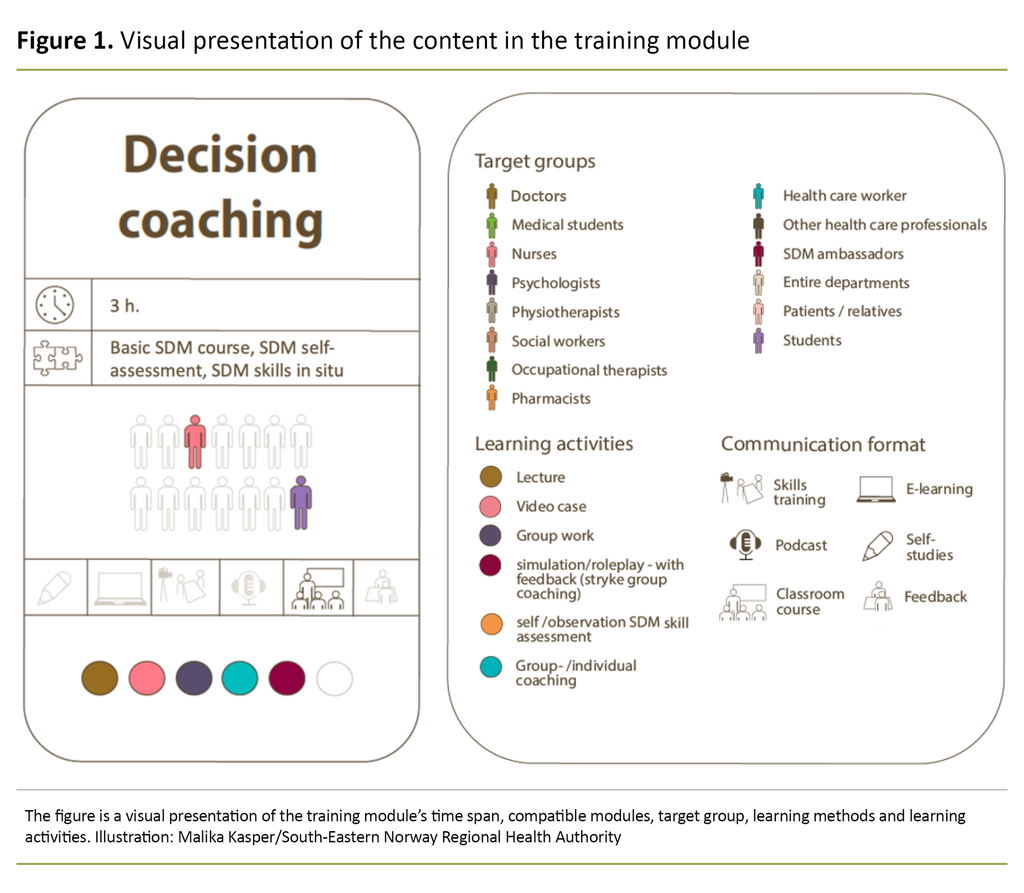
Through various teaching methods such as lectures, exercises, practical video examples and group discussions, students form an overview of the background and rationale for SDM, the situations in which it is relevant and the role of the RN (Figure 1).
Moreover, the training comprises evidence-based patient information (20), including risk communication, different measures to support SDM and a review of the step-wise process ‘Six steps to shared decision-making’ (Figure 2). This provides guidelines in how to structure decision-making conversations in order to promote SDM (15).
The last hour is used for skills training where the students perform role plays and work in pairs in the roles of patient and nurse/decision coach. The starting point is a healthcare-related issue occurring in their everyday clinical work that requires a decision-making process.
An SDM process is then carried out backed up by the ‘Six steps to shared decision-making’ memo card. This can be used in decision coaching, followed by a summary including dialogue, reflection and questions. Further information on the development and generic contents of several of the training modules in the ‘Ready for SDM’ framework is provided elsewhere (14, 15).
Data collection
Following the training module, the students accessed an online questionnaire on the Canvas learning platform. The questionnaire has previously been used in similar evaluations (15, 16), and the questions are formulated in line with Kirkpatrick’s model (25). The questionnaire included demographic data such as gender, age and length of clinical practice as well as 15 questions (25). A total of eight of the 15 questions had a four-point Likert response scale ((1 = ‘strongly disagree’, 4 ‘strongly agree’), one question had a three-point scale (‘yes’, ‘no’, ‘uncertain’), and there were two multiple-choice questions and four open-ended questions that were answered using free text.
Data analysis
We analysed the data using descriptive quantitative methods (mean, number, proportion [percentage]) via IBM SPSS Statistics V22.0. The Likert scales for the variables ‘engagement’ and ‘participants’ assessment of the training module’s relevance’ were calculated by computing the number and percentage for individual response categories.
We analysed statements in the free-text responses using qualitative content analysis (30). The analysis process started with three of the authors reading student responses multiple times independently of each other in order to form an overall impression. Then we categorised the answers in pre-determined categories –barriers and facilitators – for two of the questions using the COM-B model (31).
The COM-B model is part of the Behaviour Change Wheel model consisting of 19 theories that provide a basis for understanding motivation for behaviour change. The COM-B model presents behaviour as a result of an interaction between three components: capability, physical and social opportunity, and motivation.
For the other two questions, we identified the categories on the basis of the responses. Three of the authors analysed the responses individually, identifying meaning units in order to compare, discuss and select these units jointly. Finally, the content was condensed and abstracted in categories. Differences in opinion were settled through discussion at each of the stages described above.
Ethical assessments
The study was approved by the data protection officer at the South-Eastern Norway Regional Health Authority (reference number 19/00754) and approved by the respective universities. The students received a consent form together with the questionnaire, and they were informed that submission implied consent. The students could withdraw without giving a reason, and individuals would not be identified in the published material.
Results
The majority of the students were women taking a postgraduate programme in cancer nursing who worked in different professional areas (Table 2). The results of the study were reported in line with Kirkpatrick’s four-step evaluation model (25).
Level 1: The participants’ reactions
Engagement: 62 out of 76 students (82 per cent) stated that the training held their interest.
Relevance: 64 out of 76 students (84 per cent) stated that what they had learned was useful in their work at their respective workplaces.
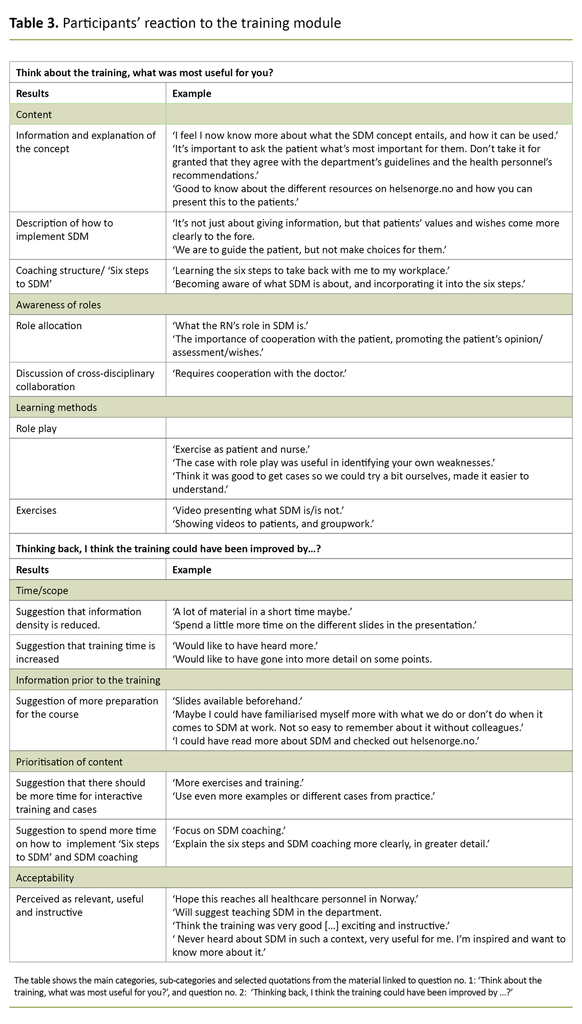
The students reported in the free-text responses that the explanation of SDM, and how decision-making conversations can be structured using ‘Six steps to SDM’, were among the most useful elements of the training. Role play, different exercises and the use of video were also highlighted as good learning methods (Table 3).
Satisfaction: 73 out of 76 students (96 per cent) stated that they would recommend the training module to other RNs. They added that it might have been useful to receive further information beforehand in order to prepare. Moreover, they would have liked the module to last longer, with more time spent on exercises and training. They found the teaching relevant, useful and instructive (Table 3).
Level 2: Participants’ learning
Subjective understanding: 65 out of 76 students (87 per cent) stated that they had understood what the term SDM entailed, 51 students (67 per cent) stated that they had understood what the term decision coaching entailed, while 25 (33 per cent) partly agreed.
Objective understanding: 65 out of 76 students (87 per cent) were able to identify the correct response to a question on the correct sequence of ‘Six steps to SDM’. Of the 76, a total of 54 students (71 per cent) chose the correct alternative in the question on what the ‘key message’ of SDM was.
Attitudes: 67 out of 76 students (88 per cent) stated that they thought it was desirable to involve patients in healthcare decisions, while 9 (12 per cent) partly agreed.
Subjective skills: 12 out of 76 students (16 per cent) stated that they had good competence decision coaching, 52 (68 per cent) partly agreed, while 12 (16 per cent) partly disagreed.
Further skills training: 69 out of 76 students (91 per cent) stated that they felt that further training would have enhanced their skills, while 7 (9 per cent) partly agreed with this.
Self-confidence: 34 out of 76 participants (45 per cent) stated that they thought it likely that they would use decision coaching as a method of supporting patients to make decisions during the next six months, 38 (51 per cent) partly agreed with this, and 3 (4 per cent) partly disagreed.
Students’ perceptions of barriers to and facilitators of the implementation of decision coaching
We used pre-determined categories to analyse the content of responses to the open-ended questions ‘What support will you need in order to make decision coaching part of the routine in the department where you work?’ and ‘What do you think may prevent you from carrying out decision coaching?’ The ‘Physical opportunity’ and ‘Social opportunity’ categories were used.
In the ‘Physical opportunity’ category, the barriers or facilitators were included in ‘Available time and resources’. These were revealed in the following quotations from students: ‘More time and opportunity to sit down and have a conversation’, and ‘The time aspect is the deciding factor but it’s possible to carry out decision coaching with good structuring and planning’.
The barrier or facilitator ‘Interprofessional collaboration and allocation of roles’ is included in the ‘Social opportunity’ category. The students expressed the following: ‘Having a memo card, bringing it up in internal training with both RNs and doctors, professional discussion internally in the department’, ‘Collaboration and agreement with colleagues, particularly doctors’, and ‘Making colleagues aware that this is something we all do’.
In the ‘Social opportunity’ category, we find ‘Organisational culture and management support’ as a barrier or facilitator, as substantiated by the following quotations: ‘Collaboration between doctors and RNs’, ‘Having an organisational culture that facilitates this’, ‘Support from management and colleagues’, and ‘Talk to the head of department about whether this is something we should focus on and implement routinely’.
Furthermore, the participants stated that they believed it was useful for several people from the same department to take part in the training together. One said: ‘Get more of my nursing colleagues involved.’ Another said: ‘Maybe I could have familiarised myself more with what we do or don’t do when it comes to SDM at work. Not so easy to remember about it without colleagues.’
In the ‘Capability’ category, the importance of ‘Knowledge, skills, access to training and support materials’ was highlighted as a facilitator.
The following quotations substantiate this: ‘Training, memo card to use in practice’, ‘Further training in coaching, clarification of how it can be implemented in the ward’, ‘Lack of knowledge about this, the goal and lots of training’, ‘I wasn’t so aware before about how to carry out SDM conversations in consultation with patients. But now I can try to use it more actively’, and ‘Include training on this during a professional development day so that we do it together’.
‘Attitudes linked to patient involvement’ were categorised as a barrier or facilitator under ‘Motivation’. The students expressed this, among other things, in the following quotations: ‘Willingness of other healthcare personnel to change their own practice, if appropriate’, and ‘But I will definitely use this when I’m a qualified cancer nurse’.
Discussion
The aim of the study was to gather knowledge about how RNs taking a master’s degree and/or a postgraduate programme respond to a three-hour training module in SDM and decision coaching, and how students perceive the effect on their learning. We also wanted to identify possible barriers to and facilitators in relation to the use of decision coaching.
The main findings in the study show that the students found the training comprehensible and useful for clinical practice. While the majority were generally positive to patient involvement in decisions about their own health as required by the SDM concept, only about half of them felt that the role of decision coach was directly relevant for them.
Need for skills training
The students said that the training module did not enhance their skills to the degree that they felt competent to use decision coaching, and said that they therefore needed more skills training. Other studies also show that more comprehensive courses are required in order to change behaviour in clinical practice (32).
The ‘Ready for SDM’ framework offers more in-depth modules that entail further skills training (14, 33).
Evaluation of the training module
A systematic overview of the evaluation methods used to evaluate SDM courses for healthcare personnel shows that Kirkpatrick’s level 1, reaction to the teaching, is the level that has been least investigated. This is the case despite the fact that participants’ positive assessment and reactions are decisive for motivation, and can therefore impact on the effect of the training. Healthcare personnel’s reported attitudes and self-confidence are the precursor to actual behaviour (34) and belong to level 2 along with knowledge and skills.
Consequently, it seems important to evaluate both levels 1 and 2 when assessing modules for competence enhancement, which are complex interventions.
SDM in health and welfare education programmes
The National Health and Hospital Plan (2020–2023) (3) specifies that SDM must be the goal and the norm. Our study helps to promote SDM by documenting a concrete training intervention in two specific postgraduate programmes. The study also shows how the ‘Ready for SDM’ framework can be used as an evidence-based approach to tailor interventions for specific groups while at the same time referencing an overarching didactic concept.
Even though SDM is incorporated into a number of health and welfare education programmes (18), SDM and health literacy should be clearly presented in the learning outcomes in the programme description of most study programmes. SDM will continue to compete with many other important topics in terms of timetabling and will probably not be allocated more time than in our training module. Therefore, it is vital that SDM is also woven into subject- specific teaching for different occupations.
Only when the concepts linked to SDM and health literacy are fully incorporated into education programmes, and the teaching conveys the importance of the patient’s autonomy, will SDM become sustainable as a best practice model.
Government investment in new strategies for the health service should be presented in study programmes. The 2020–2021 study programme for postgraduate education in cancer nursing and nephrology nursing at VID Specialized University does not include SDM. In contrast, service-user involvement and rights are mentioned as well as interprofessional interaction.
These topics fail to adequately cover legally-required SDM to ensure the patient’s participation in the choice of treatment. Postgraduate programmes in cancer nursing are being developed nationwide. It would be natural to incorporate SDM into the development of ‘RETHOS 3’, which includes education in cancer nursing, nephrology nursing and other relevant postgraduate programmes. This three-hour training model could be used as one of several interventions aimed at achieving current and future learning outcomes.
Limitations of the study
Three important limitations should be considered when interpreting the results of this study. The importance and impact of the training module should first of all be measured in light of the limited time allocated to the topic in programme descriptions and curricula. Students are expected to acquire clinical and methodological professional knowledge in a short period of time.
It is difficult to decide how much importance should be attached to generic communication skills in relation to other important learning outcomes. A three-hour training module is a good start, but no one would expect there to be a sudden and insightful increase in competence after such a short period of training.
Whether SDM can be given a more prominent position in the programme is not only a question of time but also how the topic can be credibly linked to other learning outcomes, such as knowledge about the treatment of diseases.
The study has a relatively small sample from only two different postgraduate programmes for RNs. Therefore the findings are not necessarily transferrable to other postgraduate programmes. This study was not designed to answer questions on whether the training leads to clinical behaviour changes, and thus does not cover the entire spectrum of levels in Kirkpatrick’s work.
In order to make decisions on implementation and compare the methods with the literature on competence enhancement in SDM internationally, it will be of particular importance to investigate the impact of training on the quality of communication.
Conclusion
The study shows that RNs taking a master’s degree and/or a postgraduate programme find that the training module is useful for their daily work and that they acquire good knowledge of the SDM process. Nevertheless, further training is desirable in order to strengthen RNs’ self-confidence and skills in using the method in clinical practice.
This evaluation will stimulate a review of the three-hour training module for RNs in order to make it available in other master’s and postgraduate programmes in Norway. The ‘Ready for SDM’ framework is in a process of ongoing development and has the aim of promoting the implementation of SDM. Boosting the quality and scope of SDM is a key strategic effort for the health service.
We wish to thank all the RNs who took part in the study.
The authors report no conflicts of interest.
References
1. St.meld. 34 (1996–1997). Resultater og erfaringer fra Regjeringens handlingsplaner for funksjonshemmede og veien videre. Oslo: Arbeids- og inkluderingsdepartementet; 1997. Available at: https://www.regjeringen.no/no/dokumenter/st-meld-nr-34_1996-97/id191142/ (downloaded 29.09.2022).
2. Lov 7. februar 1999 nr. 63 om pasient- og brukerrettigheter (pasient- og brukerrettighetsloven). Available at: https://lovdata.no/dokument/NL/lov/1999-07-02-63 (downloaded 22.09.2022).
3. Meld. St. 7 (2019–2020). Nasjonal helse- og sykehusplan 2020–2023. Oslo: Helse- og omsorgsdepartementet; 2019. Available at: https://www.regjeringen.no/no/dokumenter/nasjonal-helse--og-sykehusplan-2020-2023/id2679013/?ch=1 (downloaded 22.09.2022).
4. Norsk Sykepleierforbund (NSF). Yrkesetiske retningslinjer. Oslo: NSF. Available at: https://www.nsf.no/etikk-0/yrkesetiske-retningslinjer (downloaded 22.09.2022).
5. Helse- og omsorgsdepartementet. Strategi for å øke helsekompetansen i befolkningen 2019–2023. Oslo: Helse- og omsorgsdepartementet; 2019. Available at: https://www.regjeringen.no/no/dokumenter/strategi-for-a-oke-helsekompetansen-i-befolkningen-2019-2023/id2644707/ (downloaded 22.09.2022).
6. Stacey D, Legare F, Lewis K, Barry MJ, Bennett CL, Eden KB, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4(4):Cd001431. DOI: 10.1002/14651858.CD001431.pub5
7. Jull J, Köpke S, Boland L, Coulter A, Dunn S, Graham I, et al. Decision coaching for people making healthcare decisions. Cochrane Database Syst Rev. 2021;11(11):CD013385. DOI: 10.1002/14651858.CD013385.pub2
8. Couët N, Desroches S, Robitaille H, Vaillancourt H, Leblanc A, Turcotte S, et al. Assessments of the extent to which health‐care providers involve patients in decision making: a systematic review of studies using the OPTION instrument. Health Expectations. 2015;18(4):542–61. DOI: 10.1111/hex.12054
9. Kienlin S, Kristiansen M, Ofstad E, Liethmann K, Geiger F, Joranger P, et al. Validation of the Norwegian version of MAPPIN'SDM, an observation-based instrument to measure shared decision-making in clinical encounters. Patient Educ Couns. 2017;100(3):534–41. DOI: 10.1016/j.pec.2016.10.023
10. Légaré F, Adekpedjou R, Stacey D, Turcotte S, Kryworuchko J, Graham ID, et al. Interventions for increasing the use of shared decision making by healthcare professionals. Cochrane Database Syst Rev. 2018;7(7):CD006732. DOI: 10.1002/14651858.CD006732.pub4
11. Müller E, Strukava A, Scholl I, Härter M, Diouf NT, Légaré F, et al. Strategies to evaluate healthcare provider trainings in shared decision-making (SDM): a systematic review of evaluation studies. BMJ Open. 2019;9(6):e026488. DOI: 10.1136/bmjopen-2018-026488
12. Diouf NT, Menear M, Robitaille H, Guerard GP, Legare F. Training health professionals in shared decision making: Update of an international environmental scan. Patient Educ Couns. 2016;99(11):1753–58. DOI: 10.1016/j.pec.2016.06.008
13. Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95. DOI: 10.1007/s12160-013-9486-6
14. Kienlin S, Poitras M-E, Stacey D, Nytrøen K, Kasper J. Ready for SDM: evaluating a train-the-trainer program to facilitate implementation of SDM training in Norway. BMC Medical Informatics and Decision Making. 2021;21(1):140. DOI: 10.1186/s12911-021-01494-x
15. Kienlin S, Nytrøen K, Stacey D, Kasper J. Ready for shared decision making: Pretesting a training module for health professionals on sharing decisions with their patients. Journal of Evaluation in Clinical Practice. 2020;26(2):610–21. DOI: 10.1111/jep.13380
16. Kienlin S, Stacey D, Nytrøen K, Grafe A, Kasper J. Ready for SDM – evaluation of an interprofessional training module in shared decision making – a cluster randomized trial. Patient Education and Counseling. 2022;105(7):2307–14. DOI: 10.1016/j.pec.2022.03.013
17. Kasper J, Hoffmann F, Heesen C, Köpke S, Geiger F. MAPPIN'SDM – The Multifocal Approach to Sharing in Shared Decision Making (MAPPIN'SDM). PLoS ONE. 2012;7(4):e34849. DOI: 10.1371/journal.pone.0034849
18. Forskrift 15. mars 2019 nr. 412 om nasjonal retningslinje for sykepleierutdanning. Available at: https://lovdata.no/dokument/SF/forskrift/2019-03-15-412 (downloaded 22.09.2022).
19. General Medical Council. Good medical practice. London: The General Medical Council; 2013. Available at: http://www.gmc-uk.org/guidance/good_medical_practice/partnerships.asp (downloaded 22.09.2022).
20. Lühnen J, Albrecht M, Mühlhauser I, Steckelberg A. Leitlinie evidenzbasierte Gesundheitsinformation. Hamburg: Leitlinie Gesundheitsinformation; 2017. Available at: https://www.leitlinie-gesundheitsinformation.de/?lang=en (downloaded 22.09.2022).
21. Høgskolen i Innlandet. KRE4 Videreutdanning i kreftsykepleie. Elverum: Høgskolen i Innlandet. Available at: https://www.inn.no/studiehaandbok/studiehaandboeker/2020-2021-studiehaandbok/studier/hsv-fakultet-for-helse-og-sosialvitenskap/videreutdanninger/kre4-videreutdanning-i-kreftsykepleie#emnetabell (downloaded 22.09.2022).
22. VID vitenskapelige høgskole. Studieplan for videreutdanning i kreftsykepleie 2020–2021. Oslo: VID vitenskapelige høgskole; 2021. Available at: https://www.vid.no/planer/studieplan-for-videreutdanning-i-kreftsykepleie-2020-2021/ (nedlastet 22.09.2022).
23. VID vitenskapelige høgskole. Studieplan for videreutdanning i nefrologisk sykepleie 2020–2021. Oslo: VID vitenskapelige høgskole; 2020. Available at: https://www.vid.no/planer/studieplan-for-videreutdanning-i-nefrologisk-sykepleie-2020-2021/ (nedlastet 22.09.2022).
24. Reitan AM, Schjølberg TK. Kreftsykepleie, Pasient – Utfordring – Handling. Oslo: Cappelen Damm Akademisk; 2017.
25. Kirkpatrick JD, Kirkpatrick WK. Kirkpatrick's four levels of training evaluation. Alexandria, Virginia: ATD Press; 2016.
26. Stacey D, Murray MA, Légaré F, Sandy D, Menard P, O'Connor A. Decision coaching to support shared decision making: a framework, evidence, and implications for nursing practice, education, and policy. Worldviews on Evidence‐Based Nursing. 2008;5(1):25–35. DOI: 10.1111/j.1741-6787.2007.00108.x
27. Légaré F, Stacey D, Gagnon S, Dunn S, Pluye P, Frosch D, et al. Validating a conceptual model for an inter-professional approach to shared decision making: a mixed methods study. Journal of Evaluation in Clinical Practice. 2011;17(4):554–64. DOI: 10.1111/j.1365-2753.2010.01515.x
28. Knowles M. Andragogikk: en kommende praksis for voksenopplæring. In: Illeris K, Berri S, eds. Tekster om voksenlæring. Frederiksberg: Samfundslitteratur; 2005. pp. 59–72.
29. Kienlin S, Nytroen K, Kasper J, Stacey D. Shared decision-making supported by decision coaches – evaluation of a training module. Oslo: OCHER; 2020.
30. Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qualitative Health Research. 2005;15(9):1277–88. DOI: 10.1177/1049732305276687
31. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation Science. 2011;6(1):42. DOI: 10.1186/1748-5908-6-42
32. Berger-Hoger B, Liethmann K, Muhlhauser I, Haastert B, Steckelberg A. Nurse-led coaching of shared decision-making for women with ductal carcinoma in situ in breast care centers: A cluster randomized controlled trial. Int J Nurs Stud. 2019;93:141–52. DOI: 10.1016/j.ijnurstu.2019.01.013
33. Geiger F, Liethmann K, Reitz D, Galalae R, Kasper J. Efficacy of the doktormitSDM training module in supporting shared decision making – Results from a multicenter double-blind randomized controlled trial. Patient Educ Couns. 2017;100(12):2331–8. DOI: 10.1016/j.pec.2017.06.022
34. Légaré F, Freitas A, Thompson-Leduc P, Borduas F, Luconi F, Boucher A, et al. The majority of accredited continuing professional development activities do not target clinical behavior change. Acad Med. 2015;90(2):197–202. DOI: 10.1097/ACM.0000000000000543
![Figure 2. Six steps to SDM [in Norwegian only] Figure 2. Six steps to SDM [in Norwegian only]](/sites/default/files/styles/large/public/2023-01/FORSKNING_Kienlin_figur_2_ENG.png?itok=MppcCvpD)
















Comments